| |
May
2016
- Volume 10, Issue 2
The Impact of Prolonged Bed Rest After Percutaneous Coronary
Intervention in Terms of Vascular Complications and other
Patients' Outcomes

|
 ( (
|
Mohammad
Ali Abu Sa'aleek (1)
Salah Nader (2)
Mohammad Y. N. Saleh (3)
Muhammad Darawad (4)
(1)
Registered Nurse, RN at Zarqa governmental hospital,
Zarqa, Jordan
(2) Registered Nurse, RN at Al-Mafraq governmental hospital
, Al-Mafraq , Jordan,
(3) Associate Professor, Clinical Nursing Department,
University of Jordan, Amman
(4) Associate Professor, Clinical Nursing Department,
University of Jordan, Amman
Correspondence:
Mohammad Ali
Abu Sa'aleek, MS
Registered Nurse,
Zarqa Governmental Hospital, Zarqa, Jordan
The University of Jordan, Amman, Jordan
Email: Moha_blood1988@yahoo.com
|
 |
|
Abstract
Background: The use of Percutaneous Coronary
Intervention (PCI) has achieved extensive importance
in the management of Cardiovascular diseases, in order
to minimize post-PCI complications. Patients are restricted
to bed rest for various periods to prevent vascular
complications. Prolonged bed rest may accompany patient's
discomfort such as back pain, fatigue, dissatisfaction
and other patient outcomes.
Objective: The aim of this paper was to highlight
the effect of prolonged bed rest after the PCI procedure
in terms of vascular complications and other patient
outcomes, and to emphasize the importance of early ambulation
post-PCI.
Method: Descriptive design has been used with
multiple times measurement to assess the impact of prolonging
bed rest after percutaneous coronary intervention. 30
patients were selected to describe selected patients'
outcomes including low back pain, puncture site pain,
fatigue, comfort, satisfaction, urinary discomfort,
hematoma, and bleeding using visual analogue scale (VAS).
Results: This paper recommends that early ambulation
after percutaneous coronary intervention is safe and
practical, consequently leading to higher levels of
satisfaction and comfort and lower level of fatigue,
low back pain and urinary discomfort without jeopardizing
patient safety.
Key words: Early ambulation,
Patient outcomes, Percutaneous coronary intervention,
Prolonged bed rest, Vascular complications.
|
Introduction
Cardiovascular diseases
are considered the leading cause of death worldwide. They
are responsible for 30% of all global deaths (WHO, 2011) so,
there is a constant drive to develop innovative methods and
devices that enable health care professionals to achieve diagnostic
or therapeutic goals while reducing procedural related risks
and enhancing patients' satisfaction (Bechara, Annambhotla
& Lin, 2010).
Cardiovascular disease according to the American Heart Association
is defined as any abnormal condition characterized by dysfunction
of the heart and blood vessels. It includes many groups such
as cerebrovascular diseases, peripheral arterial diseases,
rheumatic heart diseases, and coronary artery diseases which
account for 42% of all global deaths that are caused by cardiovascular
diseases (WHO, 2011).
Beside drug therapy, invasive technology for the management
of coronary artery diseases has improved considerably over
the past two decades. One of these technologies is Percutaneous
Coronary Intervention (PCI) which has become a routine diagnostic
tool in cardiology departments worldwide, and has a substantial
role in the management of coronary artery diseases, and is
considered the most common invasive procedure used for this
entity (Augustin, Quadros & Sarmento-Leite, 2010; Tongsai
& Thamlikitkul, 2012; Schiks et al, 2008, Haj-Hassan,
Hamdan-Mansour, Zeilani & Nabolsi, 2013).
Percutaneous coronary intervention procedures require an arterial
access to reach coronary arteries and cardiac chambers and
that is performed by insertion of device called a sheath in
the selected artery. Although the procedure is generally safe,
many vascular complications after removing of sheath do occur
(Line, Guffey, VanRiper & Kline-Rogers, 2006).
In the USA; 3% of patients experience vascular complications
after percutaneous coronary intervention (Dumont, 2007). These
complications range from bleeding, ecchymosis, and hematoma
(Sabo, Chlan & Savik, 2008) to more serious pseudoaneurysms
and arteriovenous fistula (Konstance et al, 2004). Keep in
mind that these vascular complications are responsible for
increasing morbidity, length of stay, increase patient distress,
and decrease patient comfort (Pracyk et al, 1998 & Konstance
et al 2004).
Since the most common arterial access used in percutaneous
coronary intervention procedures is femoral artery; effective
control of femoral arterial access has received intense focus
in the past decades (Hassan, Hasan-Ali & Ali, 2013; Bechara
et al, 2010).
Traditionally, immobilization including prolonged bed rest
for six hours or more after percutaneous coronary intervention
has been used to reduce vascular complications (Schiks et
al, 2008), but this prolonged bed rest reveals on the other
hand, many complications related to patients' comfort level
and general well-being (Chair, Ya, Choi, Wong, Sit &Ip,
2012).
Prolonged bed rest for six hours or more after percutaneous
coronary intervention leads to increase the level of low back
pain and urinary discomfort, and decrease the level of comfort
and general well-being (Augustin et al, 2010 & Chair et
al, 2012). Keep in mind that these complications contravene
the international attempts to achieve diagnostic or therapeutic
goals for percutaneous coronary intervention while reducing
procedural related risks and enhancing patients' satisfaction
(Bechara et al, 2010).
Cardiovascular diseases (CVD) are defined according to the
World Health Organization as a group of disorders of the heart
and blood vessels. It includes coronary heart disease, cerebrovascular
diseases, peripheral arterial diseases, and congenital heart
disease. Cardiovascular diseases cause more than half of all
deaths across the European Region (WHO, 2014).
Invasive diagnostic tests such as cardiac catheterization
and other interventional procedures such as percutaneous transluminal
coronary angioplasty (PTCA) are becoming done widely across
cardiology departments (Haj-Hassan et al, 2013). Since their
introduction in the 1970s, the number of percutaneous coronary
intervention procedures has increased noticeably (Schiks et
al, 2008). The procedures include insertion of different sized
pieces called sheaths to femoral or radial artery to gain
an access to the vascular system (Haj-Hassan et al, 2013)
Then the cardiologist will inject special dye to allow for
exploration of coronary circulation under X-ray guidance.
However, the femoral site is considered as the most common
site due its large diameter and easier accessibility, but
unfortunately, it has higher complication (Nathan & Rao,
2012), therefore, there is an urgent need to develop ways
and plans to reduce such complications, for reducing procedure
related risks and increasing level of patient's satisfaction.
In post percutaneous coronary intervention, the complications
are not infrequently reported. It has been outlined widely
in the literature, that those complications include hematoma
at puncture site (Stone & Campbell, 2012; Cosman, Arthur
& Natarajan, 2010; Anderson, Bregendahl, Kaestel, Skriver
& Ravkilde, 2005; Sabo, Chlan & Savik, 2008) and bleeding
(Schiks et al, 2008; Cosman et al, 2010; Anderson et al, 2005;
Chair et al, 2012; Rezaei-Adaryani, Ahmadi, Asghari-Jafarabadi,
2009).
The definition of hematoma varies across research articles;
moreover its way of measurement is vague as well. Stone and
Campbell (2012) mentioned this unclear issue, while Cosman
et al (2011) reported that hematoma at vascular site is the
most frequent complication. The authors defined hematoma as
an area of swelling of the underlying tissue at the vascular
access site with or without associated bruising. Andersen
et al ( 2005) stated that hematoma development is the most
frequent complication for patients who underwent percutaneous
coronary intervention or coronary angioplasty (CA). The aims
were to determine the frequency of hematoma after percutaneous
coronary intervention and coronary angioplasty, and to identify
the predictors of its development. They include 463 subjects,
of these 322 patients underwent coronary angioplasty, and
141 underwent percutaneous coronary intervention. From a total
of forty -one patients who develop hematoma, 6 patients (1.3%
)_developed hematoma larger than 10 cm, while 35 (7.6%) developed
hematoma between 5-10 cm, moreover, the percentage of hematoma
in coronary angioplasty group was 7.5 % which is less than
percutaneous coronary intervention group (12.1%).. Further
the most statistically significant risk factor was multi artery
puncture (more than one time ) which had odds ratio ( 3.4)
and confidence interval CI ( 1.4-8.0) .The development of
hematoma due to this risk factor was 1.7, and 7.9 for coronary
angioplasty and percutaneous coronary intervention respectively.
Other risk factors include female gender and use of low molecular
weight heparin (LMWH).
Sabo et al (2008) tried to if determine patient's characteristics
and co-morbidities contributed to vascular complications.
The outcomes confirmed the previous study, that being female
is associated with higher incidence of vascular complication.
In addition, the body surface area was also statistically
significant to hematoma development among percutaneous coronary
intervention patients, odds ratio equal to 0.88 and 95% CI
equal to (0.80-0.98)
The other most commonly seen complication was bleeding from
the puncture site. Chair et al (2012) defined significant
bleeding as "blood loss estimated at greater than 100
ml or bleeding that lead to further attempts to reestablish
homeostasis by manual pressure", whereas, Schiks et al
(2008) described bleeding as any loss of blood from puncture
site needed for prolong bed rest or compression.
Moreover, Rezaei-Adaryni et al (2009) measured the bleeding
by measuring the surface area of blood at the dressing site
using a two dimensional ruler with 1 cm precision.
To reduce the complications (hematoma and bleeding) manual
hard compression by nurses or using mechanical applications
over puncture site is needed. Further, bed rest in the supine
position for 2 to 24 hours is advised. Nevertheless, the length
of bed rest after percutaneous coronary intervention varies,
and may fluctuate from 2 to 24 hours. Prolonged bed rest without
movement in the supine position is uncomfortable for most
of the patients (Chair et al, 2012).
Due to such practices (manual compression and prolonged bed
rest), most patients have some complaints or discomforts such
as low back pain, urinary discomfort, low level of comfort,
puncture site pain, low level of patient satisfaction (Chair
et al, 2012; Rezaei-Adaryani, 2009). Those complaints have
been outlined in recent literature (Sabo et al, 2008; Chair
et al, 2012; Rezaei-Adaryani, 2009; Chair, Li & Wong,
2004; Augustin et al, 2010).
According to Chair et al (2004), back pain is common among
post cardiac catheterization patients, and explained that
this is due to prolonged bed rest ranging from 3- 24 hours.
In their study, the authors aimed to identify factors associated
with back pain after percutaneous coronary intervention. They
found that turning privilege (hourly positioning to supine,
right lying, left lying related to lower level of back pain
(p = 0.001), as well as age. The older subjects reported lower
level of pain compared with younger ones. (p = 0.04) Finally,
with p value equal to 0.006, the body weight was statistically
significant, which means that the back pain is more frequent
in heavier subjects.
In a randomized control trial (RCT) done by Augustin et al
(2010) in Brazil, the results uncovered that the shorter bed
rest was better than prolonged bed rest regarding back pain.
The pain was reported in 22% versus 39% (p = 0.001), for shorter
bed rest and prolonged bed rest respectively.
Understanding factors that are related to low back pain post
percutaneous coronary intervention may help the nurses to
apply appropriate nursing intervention to improve and promote
patients' comfort (Chair et al, 2004).
Another randomized control trial was done by Rezaei-Adaryani
et al (2009) to assess the effect of changing position and
early ambulation on specific patient outcomes including level
of comfort, satisfaction, and fatigue. Patients' outcomes
were assessed after percutaneous coronary intervention six
different times., The results revealed that the level of comfort,
satisfaction and fatigue were statistically significant with
p value less than 0.001. The authors conclude that longer
duration in bed after percutaneous coronary intervention,
showed lower level of comfort and satisfaction, and the level
of fatigue was be higher.
Urinary discomfort is another patient complaint. Chair, Thompson
& Li (2007) stated that most patients have uneasiness
to urinate in bed while they are in a supine position using
urinal or bedpan. The authors compared the level of urinary
discomfort between patients who ambulated at 4 hours and 12-14
hours after cardiac catheterization Further, the results revealed
that both groups were statistically different on urinary discomfort
(p =0.006). They conclude that prolonged bed rest will result
in higher level of urinary discomfort. Five years later, a
study done by Chair et al (2012) confirmed the previous result.
In conclusion, vascular complications are common among patients
undergoing percutaneous coronary intervention; multi artery
puncture and female gender were mentioned repeatedly in the
literature as risk factors. Patient outcomes such as back
pain, urinary discomfort, satisfaction and comfort have been
assessed frequently, especially in the first few hours that
fellow percutaneous coronary intervention. The optimal bed
rest time varies across literature, because prolonged bed
rest can negatively affect those outcomes, a lot of studies
confirm the safety of early mobilization compared to late
mobilization in terms of bleeding and hematoma, in addition
to better patient outcomes.
Understanding these complications and patients' outcomes may
help nurses and other health care providers afford the patients
with suitable nursing interventions individually (Chair et
al, 201) without jeopardizing patient safety.
Significance of the study
Percutaneous coronary intervention is widely used for diagnosis
and management of cardiac diseases and considered a key clinical
tool for this entity (Augustin et al 2010; Tongsai et al 2012;
Schiks et al, 2008, Haj-Hassan et al, 2013). This produces
many serious vascular complications (Line et al 2006). One
method to prevent these vascular complications is prolonged
bed rest (Schiks et al, 2008), but this affects negatively
on patient comfort level and general well-being (Augustin
et al, 2010 & Chair et al, 2012). These factors motivated
health care professionals for many years to establish a protocol
after percutaneous coronary intervention considering patient
comfort as well as patient safety(Bechara et al, 2010). Therefore
this study is extending global studies that aimed to establish
such a protocol.
Keep in mind that it is important to base nursing practices
on high level evidence to improve the care given to individuals
undergoing percutaneous coronary intervention, so nurses need
to engage in developing evidence to support guidelines (Rolley,
Davidson, Salamonson, Fernandez & Dennison, 2008).
The results of this study will be used in building of evidence
based practice that aims to improve patient outcomes after
percutaneous coronary intervention which will be reflected
positively on patients as well as the health care system in
Jordan.
The purpose of the study
The purpose of this study is to investigate the impact of
prolonged bed rest after percutaneous coronary intervention
on patients' outcomes.
Research questions
• Is prolonged bed rest after percutaneous coronary intervention
considered a golden method to prevent vascular complications?
• What is the effect of prolonged bed rest after percutaneous
coronary intervention on other patient outcomes?
Methodology
Design
Descriptive design has been used with multiple times measurement.
The main purpose of using this design is to assess the impact
of prolonging bed rest after percutaneous coronary intervention
on patients' outcomes (low back pain, puncture site pain,
fatigue, comfort, satisfaction, urinary discomfort, hematoma,
and bleeding).
Setting
This study has been conducted in the Jordan University Hospital.
Sampling
The target population was all Jordanian patients who underwent
percutaneous coronary intervention, while the accessible population
was all Jordanian patients who underwent percutaneous coronary
intervention in the Jordan University Hospital. Convenience
sampling has been used for a select 30 participants who met
the inclusion criteria.
Inclusion criteria was any patient age of 18 years or older
who underwent diagnostic percutaneous coronary intervention
via femoral approach and received a dose of unfractionated
heparin (100 unit\kg) during the procedure.
While the exclusion criteria was any patient with aortic failure,
use of low molecular weight heparin, unfractionated heparin,
or glycoprotein IIb\IIIa inhibitors within the previous 24
hours before the procedure or after the procedure; those who
had history of hemorrhagic diathesis (bleeding tendency),
had a history of chronic low back pain, had diastolic or systolic
blood pressure higher than 100 and 180 mm Hg respectively
pre or post procedure, or who developed any vascular complications
during percutaneous coronary intervention.
Instruments
Six instruments have been used in this study, These instrument
are five Visual Analogue scales (VASs); each one consisting
of a 100-mm long line, and two dimensional ruler with 1 cm
precision.
Five Visual Analogue Scales, each one consisting of a 100-mm
long line was used to assess the following subjective data:
low back pain, puncture site pain, fatigue, comfort, satisfaction,
and urinary discomfort.
The Visual Analogue Scales consist of a 100-mm long line with
the left anchor representing "no pain, n fatigue, no
comfort, no satisfaction, no urinary discomfort", and
the right anchor representing "the worst possible pain,
the highest possible fatigue, the highest possible comfort,
the highest possible satisfaction, the highest possible urinary
discomfort". Keep in consideration that Visual analogue
scale is frequently used to assess subjective feelings such
as pain, comfort, and fatigue (Rezaei-Adaryani et al, 2009;
Chair et al, 2007).
Also, a two dimensional ruler with 1 cm precision was used
to measure the hematoma and bleeding; this method is frequently
used in the literature ((Rezaei-Adaryani et al, 2009; Chair
et al, 2007).
Hematoma was detected by observing the presence of skin discoloration
at the puncture site then measuring the distance between its
borders with this ruler, and bleeding was detected by observing
the dressing on the puncture site then measuring the distance
between its borders with the same ruler.
Data collection procedure
For eligible patients who underwent percutaneous coronary
intervention; demographic data which included gender, age,
smoking status, weight, and height were collected firstly
Secondly, the patient was assessed after two hours of bed
rest for the following variables (level of low back pain,
level of puncture site pain, level of fatigue, level of comfort,
level of satisfaction, level of urinary discomfort, amount
of hematoma if present, and amount of bleeding if present).
Keep in consideration that this assessment aimed to make baseline
information about the patient's outcomes.
Thirdly, the same variables were assessed again after four
hours of bed rest, and finally, the same variables were assessed
again after six hours of bed rest.
Ethical consideration
This study has been approved by the academic research committee
of the faculty of nursing in the University of Jordan; also
it was approved by the institutional review board of the Jordan
University Hospital. Furthermore, consent form was signed
by all participants before the beginning the study, and data
collector informed the subjects that the information will
be used for the purpose of this study only, and that was explained
to all subjects before beginning the study.
The subject was assured that he or she has the right to refuse
participation or to withdraw from the study any time; all
information will be kept in a locked cabinet at the facility
of nursing, with researcher having sole access alone, through
which the above confidentiality will be maintained.
Data analysis plan
Data analysis was carried out using the Statistical Package
for the Social Science, SPSS 16.0 for windows. Descriptive
analysis (mean, frequency, and percentage) were used for analyzing
the demographic data In addition paired-samples T test was
used to detect if there was a significant difference between
the means of the variables that were assessed after four hours
of bed rest and the means of the variables that were assessed
after six hours of bed rest.
The result
Demographic data:
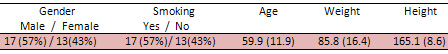
A total of 30 subjects participated in this study. Table 1
shows the demographic data. The mean age of the subjects was
59.9 years; 57% of subjects were male and 43% were female
the mean of their weight was 85.8 kg and height 165.1cm. Finally
around 57% were smokers.
Table 1: Demographic data of participants (N=30).
Comparison of the patients' outcomes
at different time intervals:
This comparison presented in Table 2 shows the mean values
of the patients' outcomes at three different time intervals,
at 2, 4, and 6 hours after bed rest respectively.
Table 2: Comparison of the patients' outcomes at three
different time intervals (N=30).
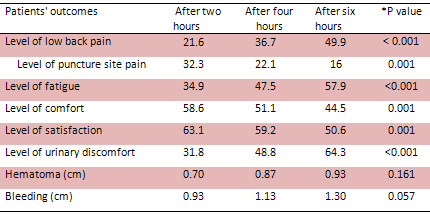
*: The p values refer to the difference between the four and
the six hour only.
The level of low back pain increased between the three intervals
considerably. This increase was statistically significant
between the second interval (4 hours) mean value equal to
36.7 and the third interval (6 hours) mean value equal to
49.9, with p value less than 0.001. Moreover, the level of
fatigue also increased markedly among the three different
intervals, which was also statistically significant between
the second interval (4 hours) mean value equal to 47.5 and
the third interval (6 hours) mean value 57.9 with p value
less than 0.001. Finally, urinary discomfort also increased,
which was also statistically significant between the second
interval (4 hours) mean value equal to 48.4 and the third
interval (6 hours) mean value equal to 64.3, with p value
less than 0.001.
The puncture site pain decreased among different intervals,
ranging from 32.3 to only 16. The satisfaction level is decreased
among the three intervals. This reduction was statistically
significant between the second interval (4 hours) mean value
equal to 59.2 and the third interval (6 hours) mean value
equal to 50.6, with p values equal to 0.001. Moreover, the
comfort level is decreased among the three intervals. This
reduction was statistically significant between the second
interval (4 hours) mean value equal to 51.1 and the third
interval (6 hours) mean value equal to 44.5 , with p values
equal to 0.001.
The patients as expected, experience vascular complications
such as bleeding and hematoma, but the occurrence of those
vascular complications were not statistically significant
among the second and third intervals.
Discussion
Previous study showed that extended bed rest in the supine
position is hard for many patients who have undergone percutaneous
coronary intervention (Chair et al., 2003). The results of
this study showed that regarding the levels of low back pain,
fatigue and urinary discomfort, there were significant differences
between the second and third intervals.
The main findings of this study were that the amount of patient
outcomes are related to the duration of bed rest. The longer
the patients are required to remain in complete bed rest in
supine position after percutaneous coronary intervention without
ambulation, the higher the levels of low back pain, fatigue
and urinary discomfort they will experience.
On the other hand, the results of this study revealed that
regarding the puncture site pain, satisfaction and comfort
level, all are decreasing with time. There were statistically
significant differences between the second and the third intervals.
We can conclude that the longer the patients are required
to remain in complete bed rest in supine position after percutaneous
coronary intervention without ambulation, the lower the puncture
site pain, satisfaction and comfort level they will experience.
This conclusion has been confirmed previously by Reazaei-Adaryani
et al (2009).
The findings also show that the patients experience vascular
complications at the puncture site such as bleeding and hematoma,
but these findings did not statistically significantly increase
or decrease between the second and the third intervals. This
result agrees with the previous literature that confirmed
no difference in comparing of vascular complications among
patients with early versus late ambulation.
Implementation
The findings of this study will be used in two approaches;
research and practice. These finding will help the researcher
to investigate more about these complications, and these findings
also will help the nurses to develop evidence-based policy
regarding bed rest post percutaneous coronary intervention,
instead of anecdotal evidece.
Limitation
The first limitation in this study is the design, so we recommend
performing further studies with more powerful design (e.g.,
randomized controlled trial). The second limitation in this
study is the sample and setting, with small sample size, so
we recommend enlarging the sample and enroll more hospitals
in future studies.
Conclusion and recommendations
Based on the statistically significant results, we recommend
early mobilization after percutaneous intervention, rather
than late, which is not common in Jordanian hospitals in general.
This change in practice aims to alleviate some patients' outcomes
such as low back pain, fatigue, and urinary discomfort, in
addition to improving the level of comfort and satisfaction.
Also the new proposed change will not affect the levels of
both bleeding or hematoma or jeopardize patient's safety.
To sum up, the longer the patients are required to remain
in complete bed rest in supine position after PCI without
ambulation, the higher the levels of low back pain, fatigue
and urinary discomfort, and the lower level of satisfaction
and comfort, without affecting the level of hematoma and bleeding.
References
Andersen, K., Bregendahl, M., Kaestel, H., Skriver, M. &
Ravkilde, J. (2005). Hematoma after coronary angiography and
percutaneous coronary intervention via the femoral artery-frequency
and risk factors. European Journal of Cardiovascular Nursing,
4, 123-127.
Augustin, A., Quadros, A. & Sarmento-Leite, R. (2010).
Early sheath removal and ambulation in patients submitted
to percutaneous coronary intervention: a randomized clinical
trial. International Journal of Nursing Studies, 47, 939-945.
Bechara, C., Annambhotla, S. & Lin, P. (2010). Access
site management with vascular closure devices for percutaneous
transarterial procedures. Journal of Vascular Surgery, 52(6),
1682-1696.
Cardiovascular disease statistic from World Health Organization
web site:
www.who.int.
Chair, S. Yu, M., Choi, K., Wong, E., Sit, J., Ip, W. (2012).
Effect of early ambulation after transfemoral cardiac catheterization
in Hong Kong: a single-blinded randomized controlled trial.
The Anatolian Journal of Cardiology, 12, 222-230.
Chair, S., Fernandez, R., Lui, M., Lopez, V. & Thompson,
D. (2008). The clinical effectiveness of length of bed rest
for patients recovering from trans-femoral diagnostic cardiac
catheterization. International Journal of Evidence-Based Healthcare,
6, 352-390.
Chair, S., Li, K. & Wong S. (2004). Factors that affect
back pain among Hong Kong Chinese patients after cardiac catheterization.
European Journal of Cardiovascular Nursing, 3, 279-85.
Chair, S., Taylor-Piliae, R., Lam, G. & Chan, S. (2003).
Effect of positioning on back pain after coronary angiography.
Journal of Advanced Nursing, 42(5), 470-478.
Chair, S., Thompson D. & Li, S. (2007). The effect of
ambulation after cardiac catheterization on patient outcomes.
Journal of Clinical Nursing, 16, 212-214.
Chair, S., Yu, M., Choi, K., Wong, E., Sit, J. & Ip, W.
(2012). Effect of early ambulation after transfemoral cardiac
catheterization in Hong Kong: a single-blinded randomized
controlled trial. The Anatolian Journal of Cardiology, 12,
222-230.
Cosman, T., Arthur, H. & Natarajan, M. (2010) .Prevalence
of bruising at the vascular access site one week after elective
cardiac catheterization or percutaneous coronary intervention,
Journal of Clinical Nursing, 20, 1349-1356
Dumont, C. (2007). Blood pressure and risks of vascular complications
after percutaneous coronary intervention. Dimens Crit Care
Nurs, 26(3), 121-127.
Haj-Hassan, A., Hamdan-Mansour, A., Zeilani, R. & Nabolsi,
M. (2013). Femoral sheath removal after cardiac catheterization
in Jordanian hospitals: an explorative study, Health, 5(3),
462-431.
Hassan, A., Hasan-Ali, H. & Ali, A. (2013). A new femoral
compression device compared with manual compression for bleeding
control after coronary diagnostic catheterizations. The Egyptian
Heart Journal.
Nathan, S. & Rao, S. (2012). Radial versus femoral access
for percutaneous coronary intervention: Implications for vascular
complications and Bleeding, Current Radiology Reports, 14,
502-509.
Pracyk, J. Wall, T., Longabaugh, J., Tice, F., Hochrein, J.,
Green, C., …, Tcheng, J. (1998). A randomized trial of
vascular hemostasis techniques to reduce femoral vascular
complications after coronary intervention. The American Journal
of Cardiology, 81, 970-976.
Rezaei-Adaryani, M., Ahmadi, F. & Asghari-Jafarabadi,
M. (2009). The effect of changing position and early ambulation
after cardiac catheterization on patients' outcomes: a single-blind
randomized controlled trial. International Journal of Nursing
Studies, 46, 1047-1053.
Rezaei-Adaryani. M., Ahmadi, F., Mohamadi, E. & Asghari-Jafarabadi,
M. (2009). The effect of three positioning methods on patient
outcomes after cardiac catheterization. Journal of Advanced
Nursing, 65(2), 417-424.
Rolley, J., Davidson, P., Salamonson, Y., Fernandez, R. &
Dennison, C. (2009). Review of nursing care for patients undergoing
percutaneous coronary intervention: a patient journey approach.
Journal of Clinical Nursing, 18, 2394-2405.
Sabo, J., Chlan, L. & Savik, K. (2008). Relationships
among patient characteristics, comorbidities, and vascular
complications post-percutaneous coronary intervention. Heart
and Lung, 37(3), 190-195.
Schiks, I., Schoonhoven, L., Aengevaeren, W., Nogarede-Hoekstra,
C., Achterberg, T. & Verheugt, F. (2008). Ambulation after
femoral sheath removal in percutaneous coronary intervention:
a prospective comparison of early vs. late ambulation. Journal
of Clinical Nursing, 18, 1862-1870.
"Stone, P. & Campbell, J. (2012).Complications related
to femoral artery access for transcatheter procedures. Vascular
and endovascular surgery, 46,617-622
Tagney, J & Lackie, D. (2005). Bed-rest post-femoral arterial
sheath removal-what is safe practice? A clinical audit. Nursing
in Critical Care, 10(4), 167-173.
Tongsai, S. & Thamlikitkul, V. (2012). The safety of early
versus late ambulation in the management of patients after
percutaneous coronary interventions: a meta-analysis. International
Journal of Nursing Studies, 49, 1084-1090.
World Health Organization Website (Europe)
http://www.euro.who.int/en/health-topics/noncommunicable-diseases/cardiovascular-diseases/cardiovascular-diseases2/definition-of-cardiovascular-diseases
|
 |




