| |
June
2013 - Volume 7, Issue 3
Changes in
cognitive and functional status of the hospitalized elderly
and their related factors: a cross-sectional study

|

(
|
Shahin Salarvand (1)
Yadollah Pournia (2)
(1) Instructor; Faculty
Member of Hepatitis Research Center, Lorestan University
of Medical Sciences, Khorramabad, Iran
(2) Instructor, Faculty of Medicine, Lorestan University
of Medical Sciences, Khorramabad, Iran
Correspondence:
Shahin Salarvand
Instructor; Faculty Member of Hepatitis Research Center,
Lorestan University of Medical Sciences, Khorramabad,
Iran
Email:
shsalarvand@gmail.com; shsalarvand@lums.ac.ir
|
 |
|
Abstract
Introduction: Since
desirable cognitive and physical performances are vital
factors to promote and preserve the quality of life
for the elderly, the present study was conducted to
investigate concurrent changes in functional and cognitive
status of the hospitalized elderly and their related
factors.
Materials and Methods:
This descriptive cross-sectional study was conducted
with a sample size of 400 people chosen through availability
sampling. The data was collected through two questionnaires.
The first questionnaire consisted of two parts, including
the demographic characteristics and the 6-Item Cognitive
Impairment Test (6CIT), and the second questionnaire
was the Barthel Index.
Results: The results
showed significant relationships between disease diagnosis
and age with cognitive status, between age and diagnosis
type with functional status, and between functional
decline and cognitive status in daily activities of
the elderly. Moreover, the odds ratio of unhealthy cognitive
status in the elderly with functional decline (or dependent
functional status) was about 8 times the ratio in the
independent functional status.
Conclusion: There are
concurrent changes in functional status in daily activities,
and cognitive status of the hospitalized elderly. This
study showed that 8 out of 10 of the hospitalized elderly
patients suffered from varying degrees of undesirable
cognitive status.
Key words: functional status, cognitive status,
elderly, hospital
|
Introduction
In mid-2004, about 10% of the world population, namely 606
million people, were aged 60 years or older (1), and this
number will exceed 1.1 billion people by 2025 (2). According
to the 2007 census in Iran, this country has become an old
country, having more than 7.2% of the elderly aged over 60
(3). Determining care priorities in this group is of great
importance because of their visits to emergency departments
for medical treatment, and their costly health care, therapy,
and rehabilitation services (4). Care and concern for the
elderly cannot be limited to a single principle, but it can
be implemented optimally through joint efforts (5). Demographic
studies have shown that approximately 5% of people aged 65
and over suffer from significant cognitive impairments. The
incidence of the disorder after the age of 65 doubles every
five years, so that it exceeds 40% in the population aged
80 years old and over (6). In addition, it is estimated that
the number of elderly with functional decline will nearly
triple by 2050 (3). Physical and cognitive performance disorders
represent two of the most frightening conditions in the elderly
because they can lead to physical dependence and social isolation
(7). Melzer, as mentioned in Adibhajbagheri et al., states
that one-third of the elderly suffer from cognitive impairment,
and more than 60% of them need help in their daily activities
(8). The multi-dimensional nature of physical performance
emphasizes the complexity of its investigation. The connected
nature of physical and cognitive performances highlights the
importance of cognition in investigating physical performance
in the elderly (7). On the other hand, hospitalization has
been identified as a critical event in the life of the elderly
(9), and optimal cognitive performance is a crucial factor
for improving and maintaining the mental health and life quality
of the elderly (10). Psychological evaluation is performed
to determine the quality of elderly people's consciousness
and awareness of their environment, and the levels of their
confusion, delirium, or dementia (11). In addition, patients
with impaired cognition on admission have less compatibility
with the risks associated with hospitalization, show less
willingness for medical treatment, and tend to have more problems
in reporting drug side effects (12). The risk of functional
decline or disability is also higher in elderly patients because
hospital environments are not often compatible with the special
needs of this population (9). On the other hand, determining
the overall score for daily living activities and level of
independence in these activities is important, can determine
the overall health status of an elderly person, and can function
as an appropriate guide to provide classification and type
of services for the elderly (13). The goal of nursing is to
maintain and enhance the functional status of the elderly
and to help them in identifying and applying their abilities
in order to achieve optimum independence (5). The elderly
people need constant care and supervision when they lose their
abilities to perform their simple daily activities (14), and
the nurse helps them to maintain their personality and maximize
their independence (5). Therefore, the assessment of cognitive
and physical performance in hospitalized elderly patients
is essential, and it is hoped that the results of the present
study will be effective in improving care programs in hospitalized
elderly patients. The present study was conducted to investigate
the coincident changes in functional and cognitive status
in hospitalized elderly people and their related factors.
Materials
and Methods
This descriptive, cross-sectional (correlational) study was
conducted with a sample size of 400 persons in 2012. After
the official permissions were taken from Lorestan University
of Medical Sciences, Iran, for visiting the hospital, the
sampling was performed through the availability sampling method.
The data collection was performed with the joint help of two
questioners (nurses). All the elderly patients (60 years and
over) who were admitted to the hospital wards were sampled
at one point of time. The two questioners, when aware of the
hospitalization of an elderly patient in the hospital, attended
the hospital and did the sampling through surveying the elderly
patient and completing two questionnaires. The sampling was
performed from the winter of 2011 and continued to the beginning
of the summer of 2012. All the ethical considerations were
regarded and the elderly patients unwilling to participate
in the study were excluded.
The data in this study was collected via two questionnaires.
The first questionnaire consisted of two parts including the
demographic characteristics, and the 6-Item Cognitive Impairment
Test (6CIT), and the second questionnaire was the Modified
Barthel Index. Concerning the reliability and validity of
these tools, since the 6-Item Cognitive Impairment Test (6CIT)
has been applied in various studies including in a study by
Hatfield et al., and because it does not contain any cultural
components, its reliability and validity have been confirmed
(15). The maximum score for this scale is 28. Subjects with
a score of 0-7 are of normal cognitive status, and those with
a score of 8-28 are considered to have undesirable cognitive
status or cognitive impairment. The Modified Barthel Index
is applied to assess a persons' daily performance in daily
activities, and their mobility. The index has 10 items, including
the questions related to eating, bathing, grooming, dressing,
controlling urine and feces, using the toilet, transferring
from the bed to the chair and the reverse, mobility on smooth
surfaces, and using the stairs. The major goal of this scale
is to assess the level of independence from any physical or
verbal help and for any reason, and a need for supervision
in a patient's activities signifies dependence. However, the
patients using aids such as crutches, etc. is not a barrier
to independence. The various items of this modified scale
have scores from 0 to 3, with a total of 20 scores. The Barthel
Index scoring is as follows: Scores lower than or equal to
4 are evaluated as completely dependent, scores of 5-8 as
highly dependent, scores of 9-11 as almost dependent and doing
things with help, and scores of 12 or more as completely independent.
The reliability and validity of the scale have been confirmed
in several studies (4, 16). The data was analyzed by the SPSS
17 software using descriptive statistics, the chi-square,
the Fisher's exact test, and the logistic regression models.
Results
In this study, out of a total of 400 elderly people who participated
in the study, 175 (43.8%) were male and 225 (56.2%) were female.
The mean age and standard deviation was 76.28 ± 8.3,
including 10.3% in the age range of 60-64 years, 12% in the
age range of 65-69, 13% in the 70-74 age group, 26.3% in the
75-79 age group, and 38.4% in the age range of 80 and over,
with the highest frequency in the group of 80 and over. The
study also found the reasons for the admissions to be cardiovascular
(40.3%), respiratory (26%), psychiatric (9.5%), and gastrointestinal
diseases (6.5%), respectively. Moreover, 66.8% of the patients
were hospitalized in the internal ward, 18.5% in the emergency
department, 1.5% in the eye and ear ward, 8% in the CCU, and
5.3% in the surgical ward, with the highest number of the
elderly patients in the internal ward. The data showed that
245 (61.2%) and 155 (38.8%) samples were living in urban and
rural areas, respectively.
In addition, 22.8% of the hospitalized elderly patients had
normal cognitive status, and 77.3% had cognitive impairment,
indicating the high importance of cognitive status investigation.
Additionally, 58.5% of the patients aged 60-64 years, 73.1%
of those aged 70-74 years, 75.2% of those aged 75-79 years,
and 93.5% of those aged 80 years and over had cognitive impairment.
There was a statistically significant relationship between
age and cognitive impairment (p=0.001), showing that the percentage
of cognitive impairment in the higher age groups was higher
than that in the lower age groups. Concerning functional status,
9.7% of the elderly patients were completely dependent, 4.8%
were highly dependent, 5.6% were almost dependent, and 79.8%
were completely independent.
The data presented in Table 1 shows that there were significant
relationships between cognitive status and disease diagnosis,
meaning that there was a significant difference at least between
the percentage of cognitive impairment in the patients with
cardiovascular and internal diseases, on the one hand, and
the percentage in those with respiratory or psychiatric diseases,
on the other hand. More investigation is required to understand
the relationship between cognitive status and each type of
diagnosis (Table 1). The results also showed that 79% of the
patients hospitalized in the internal ward, 74.4% of those
in the emergency department, 76.2% of those in the surgical
ward, 71.9% of those in the CCU, and 16.7% of those in the
eye and ear ward suffered from cognitive impairment, showing
a statistically significant relationship (p=0.009). The prevalence
rates of cognitive impairment, in descending order, were in
the internal, emergency, surgical, CCU, and eye and ear wards,
respectively. The chi-square test results showed that the
percentage of cognitive impairment in the eye and ear ward
was lower than that in the other wards (Table 1).
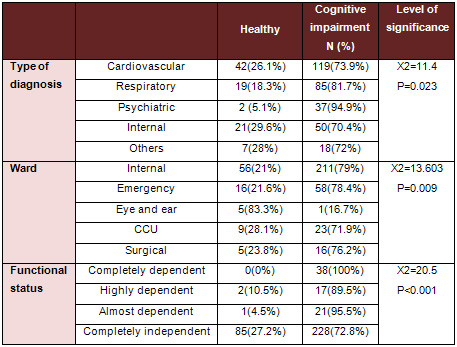
Table 1: The relationships between some characteristics
and cognitive status in the hospitalized elderly
Moreover, 62.3% of the men and 88.9% of the women suffered
from cognitive impairment, showing that the rate of cognitive
impairment in the women was significantly more than that in
the men (p <0.001). Also, 80.6% of the elderly patients
living in rural areas and 75.1% of those living in urban areas
were cognitively impaired, showing no significant difference
(p=0.198).
The vast majority of the studied population (over 99%) had
elementary school education or were illiterate, including
310 (77.5%) illiterate patients, 86 (21.5%) patients with
elementary school degrees, 1 patient with a junior high school
degree, 1 patient with a senior high school degree, and 2
with associate degrees. Therefore, assessment was not possible
in terms of educational level.
The findings showed a significant relationship between age
and functional decline (p=0.004), and the highest dependence
was for the patients in the age group of 80 and over. No significant
relationships were found between gender (p=0.902), rural and
urban place of residence (p=0.253), and type of ward (p=0.160)
with the rate of functional dependence, while a significant
relationship was found between diagnosis type and functional
status (p <0.001) (Table 2).
Click here for Table
2: The relationships between demographic characteristics and
cognitive status in the hospitalized elderly
The results presented in Table 2 show a significant relationship
between functional decline and cognitive impairment in the
elderly patients' daily activities, showing 100% of cognitive
impairment in the completely dependent patients, 95.5% in
the almost dependent ones, 89.5% in the highly dependent ones,
and only 72.6% in the completely independent patients (Table
2).
In addition, the analysis of the data showed statistically
significant relationships between cognitive status and each
of the items of the Barthel Index including eating, bathing,
transferring from the bed to the wheelchair and the reverse,
getting up from the bed, mobility, grooming (shaving, brushing,
wearing make-up, combing hair, washing the face, etc.), controlling
urine and feces, dressing, climbing up and down the stairs,
using the toilet, and bathing (p = 0.000).
The study also showed that the odds ratio of cognitive impairment
in the patients with functional decline (or dependent functional
status) was approximately 9.57 times the ratio of independent
functional status, and, on the contrary, the odds ratio of
functional decline in the patients with cognitive impairment
was 8.7 times the ratio of healthy cognitive status (Tables
3 and 4).
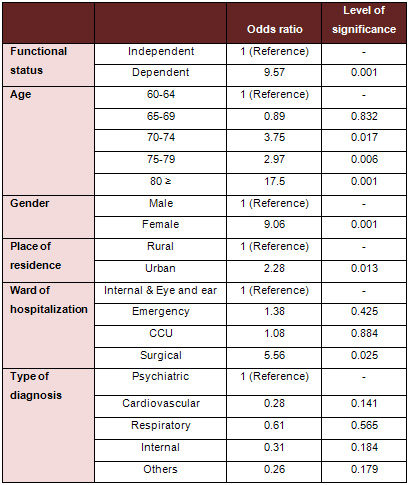
Table 3: Results of the analysis of the factors associated
with cognitive impairment using the logistic regression model
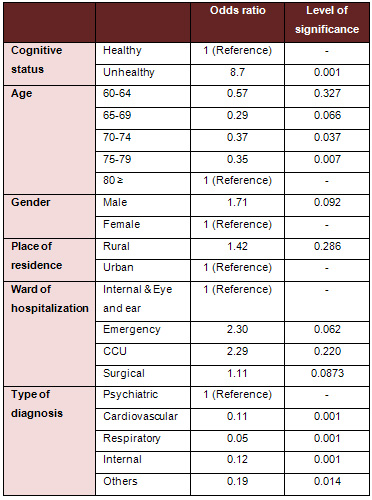
Table 4: Results of the analysis of the factors associated
with functional decline using the logistic regression model
Discussion
The findings showed that 91 of the subjects (22.8%) had scores
lower than 7 (healthy cognitive status), and 309 patients
(77.3%) had scores of 8 and over (cognitive impairment), showing
the high prevalence of cognitive impairment in the hospitalized
elderly patients. Based on a study by Taban et al., the relative
frequency of cognitive impairment ranged from 10% preoperatively
to 29.1% postoperatively (17).
Our findings showed a statistically significant relationship
between age and cognitive impairment (p<0.001), showing
a higher rate of cognitive impairment in the higher age groups
than that in the lower age groups. The results of research
by Abolghasemi et al. confirmed the finding, that aging can
affect cognitive and meta-cognitive processes significantly
and that it increases the possibility of cognitive disorders
through affecting cognitive performance (18). Taban et al's
study showed the effect of aging on increased incidence of
postoperative cognitive disorders. Most studies have considered
aging as a risk factor for cognitive impairment (17). These
studies have shown that older subjects suffer from more distraction,
weaker concentration, more memory problems, find it harder
remembering names and contents, and more oversights (18).
The results of the present study showed that cognitive impairment
in the women was significantly more than that in the men (p=<0.001).
Taban et al. revealed that there was no significant difference
preoperatively between the relative frequencies of cognitive
impairment in both genders, so that they were 9.7% in the
men and 10.4% in the women. However, the rate in the men was
more than that in the women postoperatively, showing no consistency
with the results in our study (17). In a study carried out
by Nejati et al, 3.33% of the women were found to have severe
cognitive impairment, and 18.33% and 62.13% of the men and
the women, respectively, had moderate cognitive impairment,
meaning a higher rate of cognitive impairment in the women
than that in the men, and showing consistency with our results
(12). The results of the study by Abolghasemi et al showed
that the mean score for cognitive impairment in the elderly
men was significantly higher than that in the elderly women
(18). Dirik et al's study found that the elderly men had higher
cognitive performance than the elderly women (19).
Our findings found the most common diseases in the elderly
hospitalized patients to be cardiovascular, respiratory, psychiatric,
gastrointestinal, and musculoskeletal. The most common diseases
in the elderly in Isfahan, as reported by Salarvand et al.,
were arthritis, visual impairment, and hypertension, respectively
(20). Mohtasham Amiri et al's study showed the most common
causes for admission of the elderly, to be cardiovascular
diseases, trauma, respiratory diseases, eye disorders, cancers,
cerebrovascular diseases, and infectious diseases. As mentioned
in Mohtasham Amiri et al's study, previous studies have reported
the most common causes for admission of the elderly to be
cardiovascular diseases, cancers, pneumonias, and cerebrovascular
events (2).
Our results also revealed that cardiovascular, musculoskeletal,
respiratory, psychiatric, blood, endocrine, and obstetric
diseases increased cognitive status in the elderly significantly
(p=0.049). Conducting more studies in this regard is recommended.
Gussion et al, as mentioned in Salarvand et al's study, reported
osteoarthritis, strokes, heart diseases, and depressant symptoms
as having the greatest impact on the performance of the elderly
(20). In the present study, a significant relationship was
found between cognitive impairment and ward of admission (p=0.009),
so that the highest rates of cognitive impairment were observed
in the internal, emergency, surgical, CCU, and eye and ear
wards. Moreover, no significant relationship was found between
urban and rural place of residence and cognitive impairment
(p=0.198), and no relevant studies were found in this regard.
A significant relationship was found between age and type
of diagnosis with cognitive impairment, with the highest rate
of dependence in the age range of 80 and over. Other studies
have also confirmed that aging increases the rate of severe
and moderate disabilities in the elderly (8).
In the present study, gender, urban and rural residence, and
ward were not found to have significant relationships with
functional dependence, while Dirik et al's study indicated
that the elderly women, compared to the elderly men, had a
lower level of mobility and were more dependent in their daily
activities (19). Also, Adibhajbagheri et al showed significant
relationships for age, gender, and place of residence, showing
more moderate and severe disabilities in women than in men,
more severe disabilities in cities than in suburbs, and more
moderate disabilities in suburbs than in city centers (8).
Our findings found a significant relationship between cognitive
impairment and dependence in daily activities in the elderly,
showing cognitive impairment in 100% of the completely dependent
elderly, 95.5% of the almost dependent ones, 89.5% of the
highly dependent ones, and only 72.6% of the completely independent
patients. Other studies have confirmed this finding, including
Stuck et al's study reporting a strong relationship between
cognitive impairment and functional decline (21). Also, Raj
et al's study reported that the elderly people with lower
cognitive performance had a greater chance of failure (58%
more) in the activities of daily living (ADL) (22). In Kazemi
et al's study, the more cognitive impairment the subjects
had, the lower functional scores they obtained. Therefore,
there was a significant relationship between cognitive status
and activities of daily living (23). Moreover, Arcoverde et
al found that physical activity and optimal physical performance
were associated with the lower prevalence and incidence of
dementia and cognitive impairment (24). Stuck et al showed
a strong relationship between cognitive impairment and functional
status (25).
Concerning the relationship between the components of cognition
scores and activities of daily living, the highest relationship
was found between performance activity and activities of daily
living. It confirms the finding reported by some researchers
that interference with activities of daily living possibly
occurs in more advanced stages of cognitive impairment. Yan
Hoon et al in their study concluded that functional decline
is common in nursing homes, and that more attention should
be paid to the elderly with dementia right from the admission
time (26). The findings of Dirik et al's study showed that
functional status, cognitive status, and motility decreased
in the elderly patients hospitalized in institutions (19).
Since the relationship between cognitive impairment and functional
impairment was sought in the present study, the assessment
of the relationship with drug type was not possible due to
the consumption of multiple medications by the elderly patients,
and this was one of the limitations of the present study.
The second limitation of our study was the application of
the availability sampling method, which made causative relationships
impossible.
Final conclusions
and recommendations
In this study, we investigated the concurrent changes in functional
and cognitive status of the hospitalized elderly. There was
a significant relationship between functional decline in daily
activities and cognitive impairment. The study showed that
8 out of 10 of the hospitalized elderly patients suffered
from varying degrees of undesirable cognitive status, and
this disorder was associated significantly with age, gender,
ward, type of diagnosis, and educational level. Improvements
in performance, mobility, and cognitive status should be among
the first priorities of geriatric rehabilitation, and initial
evaluation of cognitive and functional status is essential
in the assessment of the elderly in caring institutions. Independence
in functional activities and an independent life-style should
be taken into account in the elderly. Moreover, more research
is needed to identify the mechanisms that increase the vulnerability
of functional decline, and causative relationships between
impairments in physical performance and cognitive performance.
References
1. Lee TFD. Quality long term care for older people: a commentary.
Journal of Advanced nursing. 2005; 52(6): 609-619.
2. Mohtasham Amiri Z, Toloei MH, Farazmand E. Causes of patients'
hospitalization in Guilan University hospitals. J MED FAC
GUILAN UNIV MED SCIENCES. 2002; 42(11): 28-32. [In Persian]
3. Mohammadi F, Dabagi F, Yadavarenikravesh M. Facilitating
and barrier factors in fragile elders' family caring at home:
the experience of women caregivers.2007;2(6):445-453.[ In
Persian]
4. Shahhosiny S, Tagdisy H, Rahgozar M, Fadayevatan R. Relationship
between Barthel Index scoring in admission time and elders
patients' clinical findings in discharge time. Iranian Ageing
Journal.2008; 3(9, 10): 60. [In Persian]
5. Smeltzer SC. Medical-surgical nursing (Elders' diseases).
Translated by: Tabari F. Tehran, Boshra Publication; 2005.P:15.
[In Persian]
6. Frogan M, Jafari Z, Shirinbayan P, Gaem magame farahani
Z, Rahgozar M. Validation study of Mini-Mental State Examination
(MMSE) in elders living in Tehran. J Advances in Cognitive
Sciences. 2008; 10(2):29. [In Persian]
7. Tabbarah M, Crimmins EM, Seeman TE. The relationship between
cognitive and physical performance: Mac Arthur studies of
successful Aging. Journal of Gerontology Medical Sciences.2002;57A(4):
M228-M235.
8. Adibhajbageri M, Akbari H. Severity of disability and its
related factors in elders. Journal of Feyz. 2009; 13(3): 225-234.
[In Persian]
9. Pedone C, Ercolani S, Catani M, Maggio D, Ruggiero C, et
al. Elderly patients with cognitive impairment have a high
risk for functional decline during hospitalization: The GIFA
study. Journal of Gerontology: MEDICAL SCIENCES. 2005; 60A,
12: 1576-1580.
10. Nejati V, Ashayeri H. Assessing relation between cognitive
disorders and depression in elders. Iranian journal of Aging.
2006; 1(2):8-15. [In Persian]
11. Haffman G. Geriatric nursing. Translated by: Heidarali
Abedi et al: Ooroj, Isfahan University of Medical Sciences,
2003. [In Persian]
12. Miller CA. Nursing for wellness in older Adults theory
and practice. Philadelphia; Lippincott Williams & Wilkins.
2004.
13. Nejati V, Ashayeri H. Assessing relation between cognitive
disorders and depression in elders. Iranian Journal of Aging.
2006; 1(2):8-15. [In Persian]
14. Taylor F. The principles of nursing in wards. Translated
by; the faculty members of Shahid Beheshti Medical Sciences
University. Tehran: Boshra & Tohfeh; 2003. [In Persian]
15. Hatfield CF, Dudas RB, Dening T. Diagnostic tools for
dementia. Maturitas.2009; 63:181-185.
16. Karbakhshe M, Zargar M,Eshadi Z,khaji A. Mechanism and
outcome of hip fracture: a multi-center study. Tehran University
Medical Journal. 2006; 64(7):37- 46. [In Persian]
17. Taban H, Ahmadzadeh GH, Tavasoli M. Cognitive disorders
in elders before and after surgical operation. J Hormozgan
University of Medical Sciences. 2003; 7(3):136-137. [In Persian]
18. Abolgasemi A, Kiamersi A. Assessing relation between supra
cognition and cognition failure in elders. J Advances in Cognitive
Science. 2009; 11(1):8-15. [In Persian]
19. Dirik A, Cavlak U, Akdag B. Identifying the relationship
among mental status, functional independence and mobility
level in Turkish institutionalized elderly: Gender differences.
Archives of Gerontology and Geriatrics.2006;42(1):339-350.
20. Salarvand SH, Meraci M, Ghaedi F, Zamani M. Prediction
risk of falling in hospitalized elders in Esfahan, 2009. J
Kordestan University of Medical Sciences. 2010; 35(2): 25.
[In Persian]
21. Stuck AE, Walthert JM, Nikolaus T, Bula CJ, Hohman C,
Beck JC. Risk factors for functional status decline in community
living elderly people: a systematic literature review. Social
Science & Medicine.1999;48(1): 445-469.
22. Raji MA, Al Snih S, Ray LA, Patel KV, Markides KS. Cognitive
status and incident disability in older Mexican Americans:
findings from the Hispanic established population for the
epidemiological study of the elderly. Ethn Dis. 2004 winter;
14(1):26-31.
23. Kazemi H, Gasemi S, Sharifi F, Fakhrzadeh H, Gaderpanahi
M, Mirarefin M, Forogan M. Relationship between cognitive
status and functional ability in elders living in Kahrizak
nursing home. Iranian J.Aging.2009;4(12): 16-25. [In Persian]
24. Arcoverde C, Deslandes A, Rangel Az, Rangel An, Pavao
R, Nigri A, Engelhardt E, Laks J. Role of physical activity
on the maintenance of cognition and activities of daily living
in elderly with Alzheimer's disease. Arq Neuropsiquiatr.2008;
66(2-8):323-327.
25. Stuck AE, Walthert JM, Nikolaus Th, Bula CJ, Hohmann C,
Beck JC. Risk factors for functional status decline in community-
living elderly people: a systematic literature review. Social
Science & Medicine 1999; 48: 445-469.
26. Yan Hoon A, Au SYL, Yap LKP, Ee CH. Functional
decline of the elderly in a nursing home. Journal of Singapore
medicine. 2006; 47(3):219.
|
 |




