| |
June/July
2015
- Volume 9, Issue 3
Medical-Surgical Nurses' Experiences of Calling a Rapid Response
Team in a Hospital Setting: A Literature Review

|
 ( (
|
Badryah
Alshehri (1)
Anna Klarare Ljungberg (2)
Anders Rüter (3)
(1) Badryah Alshehri,
RN, BCN, Critical Care Nurse,
Sophiahemmet University, Stockholm, Sweden.
(2) (Mrs Klarare);
Anna Klarare Ljungberg: RN,MSN ,PhD,
Sophiahemmet University. Stockholm, Sweden.
(3) (Mr Rüter); Anders Rüter: MD,
Associate Professor of Surgery particular disaster medicine.
Stockholm, Sweden
Correspondence:
Badryah Alshehri,
BSN, RN, Sophiahemmet University , Spanga, 16368, Hyppingeplan16,
Stockholm, Sweden
Mobile phone: + 46765505100
Email: baa325@gmail.com
|
 |
|
Abstract
Background: The rapid response team (RRT) decreases
rates of mortality and morbidity in hospital and decreases
the number of patient readmissions to the intensive
care unit. This team helps patients before they have
any signs of deterioration related to cardiac
or pulmonary arrest. The aim of the RRT is to accelerate
recognition and treatment of a critically ill patient.
In addition, in order to be ready to spring into action
without delay, the RRT must be on site and accessible,
with good skills and training for emergency cases. It
has been reported that many hospitals are familiar with
the concept of RRTs. There is a difference between this
team and a cardiac arrest team, since the RRT intervenes
before a patient experiences cardiac or respiratory
arrest.
Aim: To describe current
knowledge about medical-surgical nurses' experiences
when they call an RRT to save patients' lives.
Method: The method used
by the author was a literature review. The PubMed search
database was used and 15 articles were selected, all
of which were primary academic studies. Articles were
analysed and classified according to specified guidelines;
only articles of grades I and II were included.
Results: Years of experience
and qualifications characterise the ability of a medical-surgical
nurse to decide whether or not to call the RRT. Knowledge
and skills are also important; some hospitals provide
education about RRTs, while others do not. Teamwork
between bedside nurses and RRTs is effective in ensuring
quality care. There are some challenges that might affect
the outcome of patient care: The method of communication
is particularly important in highlighting what nurses
need RRTS to do in order to have fast intervention.
Conclusion: Medical-surgical
nurses call RRTs to help save patients' lives, and depend
on their experience when they call RRTs. Both medical-surgical
nurses and RRTs need to collaborate during the delivery
of care to the patient. Good knowledge and communication
skills are important in delivering fast intervention
to a critically ill patient, so that deteriorating clinical
signs requiring intervention can be identified.
Key words: Medical-surgical
nurse, rapid response team, experiences, challenges,
hospital.
|
Introduction
There are some hospitals that apply plans to prevent
mortality and morbidity for patients who are critically ill,
by using guidelines to protect patients when a staff nurse
notices signs of instability before undergoing cardiac arrest
(Chan, Jain, Nallmothu, Berg, & Sasson, 2010; Butner,
2011). A nurse who is assigned
to a critically ill patient will have the chance to help the
patient to survive. Not all nurses expect that their patient
is experiencing an arrest (Dwyer & Mosel, 2002). However,
many studies have reported that the hospital staff's failure
to recognise the early signs of deterioration in patients,
such as decreasing systolic pressure and abnormal breathing,
can lead to serious concerns, such as some cases like post
surgical infection, cardiac arrest code and even death (Abella
et al, 2005; Peberdy et al., 2003).
A patient has the right to receive
good quality of care (Burkhardt & Nathaniel, 2008). Good
quality of care means improving the available health services
for individuals to achieve their desired outcomes (Vincent,
2010). Furthermore, good quality of care, from a hospital
administration's point of view, means the prevention of illness,
infection, and decreases the Intensive Care Unit (ICU) re-admissions.
It has been suggested that, in order to improve patient outcomes,
surveillance to identify problems should be linked to effective
responses (Green & Allison, 2006). To tackle this issue,
a system termed 'the Rapid Response Team' has been initiated
(Institute for Health Improvement [IHI], 2013). The Rapid
Response Team helps to decrease mortality and morbidity rates,
and also allows nurses to intervene when a patient has signs
of deterioration before they experience a cardiopulmonary
arrest (Jenkins & Lindsey, 2010).
Background
Around 60 per cent of hospitals in the US have experiences
with patients who undergo cardiopulmonary arrest (Winter et
al., 2007). Other studiesy show that most of the clinical
deterioration signs for patients are exhibited before they
reach cardiopulmonary arrest (Azzopardi, Kinney, Moulden &
Tibballs, 2011). Health care professionals have a responsibility
to know the signs of deterioration for critically ill patients
and to have responses to prevent it. Not all professional
health care workers recognise the signs that lead to death
(National Patient Safety Agency, 2007; National Confidential
Enquiry into Patient Outcome And Death, 2005). There are some
challenges that hospitals face, such as managing healthcare
workers and providing available resources, in achieving and
managing patient care and outcomes of patient services
(Rogers et al , 2004).
The Institute of Healthcare Improvement
([IHI], 2013) established in 1980 by Dr Don Berwick, works
with a group of committed individuals to re-design healthcare
into a system without delay, time consuming tasks, errors
and unsustainable costs. The IHI focuses on key aspects, including
person- and family-centred care, improvement capability, patient
safety, and quality, cost and value. The goal of the IHI is
to improve the lives of the patients and health communication.
They concentrate on safety, effectiveness, time lines, efficiency,
and equity.
Rapid Response Team: Strategies
for Saving Lives
The Institute of Health Care Improvement (2001) undertook
the initiative of the 100,000 Lives Campaign in 2004, intended
to reduce mortality and morbidity rates. This initiative's
strategyies is to implement the best practice and also to
prevent pressure ulcers, reduce methicillin-resistant Staphylococcus
aureus (MRSA) infection through control processes and policy,
reduce infection through basic changes in infection control
processes, reduce surgical complications by implementing changes
in care, and prevent harm caused by high-alert medications,
beginning with a focus on anticoagulants, sedatives, narcotics
and insulin. They achieved this goal, partly by recommending
the implementation of a Rapid Response Team (RRT).
The goal of this campaign was to save 100,000 lives during
the time from its launch in December 2004 until June 2006.
Since then they have launched a successor, the Save 5 Million
Lives Campaign. In December 2006, the Institute of Healthcare
Improvement recommended implementing the RRT as one of six
strategies used to identify patients who were experiencing
pre-arrest in unplanned ICU admission. The strategies behind
the implementation of the RRT were to bring ICU-level patient
care to the bedside of critically ill patients, to work together,
and to assess and intervene in order to save patients' lives
(Institute of Healthcare Improvement, 2013).
Currently, more than 25 per cent of US hospitals use RRTs
to decrease the incidence of cardiopulmonary arrest, re-admissions
to the ICU and deaths by providing early intervention for
patients whose conditions are acute and progressively deteriorating
(Donaldson, Shapiro, & Scott, 2009).
Different Terms for the Rapid
Response Team
It is important to understand the terminology of the Rapid
Response Teams. In the past, they were called Medical Emergency
Teams (METs) or Medical Emergency Response Teams (MERT), and
other terms including Patient at Risk Team (PART) and Critical
Care Outreach Team (CCOT) have also been used. Some of these
terms are interchangeable in places such as Australia, where
RRT and MET have the same meaning (DeVita, Hillman, &
Bellomo, 2011).
The similarity between the RRT and
the MET is that they help critically ill patients from the
emergence of any signs that could lead to cardiac or respiratory
arrest. Both maintain the two key features of an afferent
limb, such as how the team is activated, and an efferent limb,
such as the response of the team. There are, however, some
differences between them: RRT is generally used to mean a
nurse-led team, and the MET is generally a physician-led team.
In this thesis, the author will use the term 'Rapid Response
Team' to cover all of these terms, as it is the most commonly
used variant in the literature (DeVita, Bellomo, Hillman,
et al, 2006).
Definition of the Rapid Response
Team and its Purpose
DeVita et al. (2011) defined a Rapid Response Team (RRT) as
a group of healthcare professionals who are trained for critical
cases and deliver quick critical care. A RRT's members come
from multiple disciplines, including an intensivist, a physician's
assistant, a critical care nurse and a respiratory therapist.
The purpose of this team is to be
ready to spring into action without delay, and they must be
onsite and accessible;, they must have good skills and be
trained well for emergency cases (Moldenhaure, Sabel, Chu,
& Mehller, 2009).
An RRT is able to respond rapidly to a deteriorating patient
with an average response time of less than five minutes (range:
2-10 minutes), and the duration of RRT calls averages between
20 and 35 minutes (range: 5-98 minutes). A RRT is intended
to prevent hospital deaths caused by medical error in medical-surgical
wards or wherever they occur, such as in an intensive care
units (Hatler et al., 2009; Chamberlain & Donley, 2008).
Hospital Mortality and Morbidity
Numerous studies have shown the numbers of patient lives saved
when RRTs have been activated. A study in one hospital indicated
that the RRT was called 344 times over a period of 18 months.
The same study reported 7.6 cardiac arrests per 1,000 discharges
each month over a five-month period before the RRT was implemented.
However, with the introduction of the RRT, the number of cardiac
arrests over a 13-month period subsequently decreased to three
episodes of cardiac arrest per 1,000 discharges each month.
Prior to the implementation of the RRT, the mortality rate
was 2.82 per cent; after the RRT implementation, it decreased
to 2.35 per cent. Additionally, the percentage of ICU re-admissions
decreased from 45 per cent to 29 per cent (Dacey et al., 2007).
According to Bellomo et al. (2004),
the implementation of RRTs reduced adverse events in postoperative
patients, such as severe sepsis, respiratory failure, stroke,
and acute renal failure. It also reduced the duration of hospital
stays. There were 1,369 operations for 1,116 patients during
the control period and 1,313 for 1,067 patients after the
intervention of the rapid response team (RRT). The result
was a decrease in the rate of respiratory failure incidents
to 57 per cent, while the relative stroke risk reduction was
78 per cent; severe sepsis had a relative reduction of 74.3
per cent; acute renal failure requiring renal replacement
therapy relative reduction had a relative reduction of 88.5
per cent; and emergency intensive care admissions were reduced
to 66.4 per cent. Furthermore, the rate of postoperative death
dropped to 36.6 per cent, and the average duration of hospital
stays decreased from 23.8 days to 19.8 days.
DeVita et al. (2006)'s findings supported
the conclusion that the use of RRTs indeed decreases adverse
outcomes and unplanned ICU admissions, and stated that hospitals
should implement RRTs.
A recent study compared mortality
rates before and after the implementation of RRTs. It was
indicated that the initial mortality rate was 22.5 individuals
per 1,000 hospital admissions. After the RRTs were implemented,
the mortality rate dropped to 20.2 per 1,000 hospital admissions.
The utilisation of RRTs decreased the mortality rate, as well
as decreased ICU re-admission (Alqahtani et al., 2013).
Another hospital indicated that
the number of cardiopulmonary arrests before implementing
a RRT was 75 per 1,000 admissions in 2006; after implementing
the RRT, the number of cardiopulmonary arrests decreased from
59 to 37 per 1,000 admissions during 2007 and 2008 (Hijazi,
Sinno, & Alansar, 2012).
Another study found that, from 378 calls for a RRT during
a time period spanning from 9 months before until 27 months
after implementing a RRT, cardiac arrests were reduced by
57 percent, amounting to a reduction of 5.6 cardiac arrests
per 1000 hospital discharges. Around 51 arrests were prevented
(Geoffrey, Parast, Rapoport, & Wagner, 2010).
Konrad et al. (2009) found that, in a hospital where the number
of RRT calls was 9.3 per 1,000 hospital admissions, the MET
implementation was associated with a 10 per cent reduction
in total hospital mortality. The number of cardiac arrests
per 1,000 admissions decreased from 1.12 to 0.83; mortality
was also reduced for medical patients by 12 per cent, and
for surgical patients not operated upon by 28 per cent. The
30-day mortality pre-MET was 25 per cent versus 7.9 per cent
following the MET implementation compared with historical
controls. Similarly, the 180-day mortality was 37.5 per cent
versus 15.8 per cent, respectively.
The study by Scott and Elliot (2009)
showed that before implementing RRTs, 22 cardiac codes were
called per month. After implementing RRTs, this number decreased
to 14 per month. Before the implementation, the cardiac codes
were mostly called for patients who required intubation; afterwards,
the cardiac codes were seldom used for intubated patients
because the RRT had been called before the patient's condition
deteriorated.
The Criteria for and Purpose of
Calling RRTs
When the medical-surgical nurse calls the RRT, there are certain
criteria involved in the decision. When a medical-surgical
nurse notices that their patient is almost at the point of
requiring intervention, the staff nurse will review the criteria
to assess a patient before calling the RRT. Each hospital
must use certain criteria when it comes to calling RRT. The
following will help to determine who should call RRT; using
the proper protocol will help to reduce the incidence of mortality
and morbidity due to unexpected cardiac arrests in the hospital
(Buist, 2002). A study found that, through implementing RRTs,
the number of calls for RRTs increased through an understanding
of their outcome in saving patients' lives (Hillman, et al.,
2005).
Each member of the team has a role to play during an intervention.
The role of the RRT nurses is to assist the bedside nurses
and to assess patients alongside them. The role of the physician
is to assess the patient, evaluate the clinical findings in
relation to the patient's history, and to determine the appropriate
intervention with the other team members. Calling the RRT
is commonly done for surgical patients, emergency department
patients, elderly patients with multiple comorbidities, and
critically ill patients with a longer length of stay at the
hospital (Young, Donald, Parr, & Hillman, 2008). The criteria
that a nurse in a medical or surgical ward should follow in
deciding whether to call an RRT are shown in Table 1.
Table 1: The clinical criteria
for calling a RRT
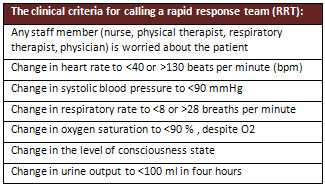
(Institute of Health Care Improvement,
2011)
The impact of implementing a RRT
is to maximise the climate of safety for a medical-surgical
patient. Promoting a more cohesive clinical approach hospital-wide,
such teams augment expertise and communication with the skills
of the nurses throughout the facility (Sharek et al., 2007).
Process for Calling a Rapid Response Team
Each hospital uses a framework for RRTs, with plans and the
mechanisms in place for a deteriorating patient. When a nurse
notices that a patient's condition is declining, after applying
the criteria, the nurse will call the RRT by pager or telephone
extension per the hospital's protocol (Institute for Clinical
System Improvement, [ICSI], 2013). The nurse will then give
a verbal report of relevant information using the communication
tool of SBAR: 'Situation' refers to the room, the ward
and a brief about the patient, including the name, age, admission
date and the reasons for admission; 'Background' covers
information about the patient's history and conditions, a
list of medications, lab results and other clinical information;
'Assessment' is the nurse's assessment of the situation;
and 'Recommendation' is what the nurse recommends,
such as whether a patient needs to be seen immediately or
needs an X-ray (Ray et al., 2009; Cretikos et al., 2006).
According to the Institute of Health
Care Improvement (2013), SBAR is an easy and effective tool
for communication about a patient between staff members.
Definition of Nursing and Nurses'
Responsibilities
Nursing is defined as protecting, promoting and optimising
health care while preventing illness and alleviating suffering
through diagnosis and treatment. Nursing is primarily concerned
with providing care to the physically ill, mentally ill and
disabled. Nursing includes collaborative care for individuals
of all ages, regardless of family, group or community, sick
or well, in all settings (International Council of Nurses,
2012).
Nurses are responsible for patient care, where each nurse
is accountable for his or her individual nursing practice,
performing assigned tasks and providing optimum care. In all
their other responsibilities, such as administration, teaching
and research, each nurse is responsible for the quality of
practice within their standard of care (American Nurse Association,
2011).
Nurses' Experience and Practice
Nurses' experience can be defined as their acquisition of
knowledge and skills from feeling, seeing and doing. Another
definition of nurses' experience is the achievement of a high
level of knowledge, work and experience relating to healthcare
from mind-body practices. Nurses' levels of understanding
evolve through their experiences of practice in clinical settings
(Kemper et al., 2011). In practice, nursing requires special
skills and knowledge, as well as independent decision-making.
Nurses must deal with different settings, types of patients,
diseases and ways of giving treatment. Nurses protect those
who need care (National Council of State Boards of Nursing,
2013).
Medical-Surgical Nurses
Nurses who work in medical and surgical wards are registered
nurses who have been professionally registered after passing
an examination to have the licence certification in order
to be qualified to perform nursing care, as well as being
equipped with the skills required to assess patients physically.
Furthermore, they have the ability to make clinical decisions
about the appropriate treatment and nursing intervention for
a patient by performing an assessment, developing a plan of
care and predicting patient outcomes (Keller, Edstrom, Parker,
Gabriele, & Kriewald, 2012).
Problem Statement
It has been reported that many hospitals
are familiar with the concept of the Rapid Response Team.
The difference between the RRT and a cardiac arrest team is
that the RRT intervenes before a patient experiences cardiac
or respiratory arrest. The RRT is a system recommended by
the Institute of Healthcare Improvement (IHI, 2010).
Significant evidence has shown that RRTs save patients' lives
by mitigating medical errors, decreasing ICU admissions, and
reducing the number of days spent in hospital (IHI, 2013).
Because of this, the author focuses on medical-surgical nurses
who are assigned to critically ill patients, who have complex
responsibilities, may struggle with lacking confidence, or
experience other challenges during RRT calls due to medical
errors. The author also seeks responses from bedside nurses
when they notice that their patient needs RRT intervention
(Thomas et al., 2007).
AIM
To describe the current knowledge
about medical-surgical nurses' experiences when they call
Rapid Response Teams to save patients' lives.
Research Questions
- How do nurses describe their experiences
of calling RRTs?
- What are the common challenges for nurses when calling RRTs?
METHOD
Study Design
A literature review is the gathering, analysis, and critical
summary of information for a particular topic of study. The
literature review is a helpful method for the researcher to
collect and condense information (Polit & Beck, 2012).
The fundamental aim of a literature review is to provide a
comprehensive picture of the existing knowledge relating to
a specific topic (Coughlan, Cronin, & Ryan, 2013). Moreover,
the use of this method helps to inspire and generate new ideas
by highlighting any inconsistencies in current knowledge,
from among studies published in some search database such
as PubMed, considered the most significant database in medicine,
and including the entire field. PubMed primarily accesses
the MEDLINE database, which includes references and abstracts.
PubMed also involves a full articles database from different
countries (Aveyard, 2010). In this study the PubMed database
was used to retrieve all articles. The vocabulary and terminology
used to search the PubMed database were found using MeSh (Medical
subject Headings), a dictionary used for indexing articles.
Data Collection
Data collection is a formal research procedure used to help
a researcher. This study performed a search to find articles
relevant to nurses' experiences during calls to RRTs. PubMed
is considered as the most significant database for this purpose
and has been used in this study (Polit & Beck, 2012).
All 15 articles retrieved from PubMed
answered the study's aim. MeSH terms were used to find some
of terminology, which was then used in a free search in PubMed.
However, there were no articles found in MeSh database related
to this topic (Polit & Beck, 2012). The terms used in
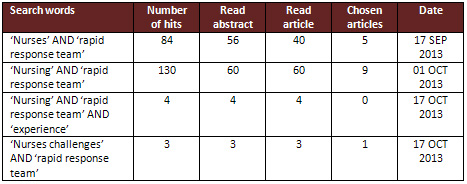
MeSh were: 'nursing' AND 'Rapid Response Team'; 'nurses' AND
'Rapid Response Team'; 'nursing' AND 'Rapid Response Team'
AND 'experience' and 'nurses'; and 'challenges' AND 'Rapid
Response Team' (see Table 2). The following inclusion and
exclusion criteria were applied during search in selecting
articles for this review.
Selection Criteria
Inclusion criteria
The inclusion criteria was to include articles, then analyse
them for use in the result (Polit & Beck, 2012). This
criteria used for each article included had to be written
in English, with a publication date no earlier than ten years
ago, and also filed under publications involving the nursing
field. These were then used as the primary source texts, original
studies and primary sources.
Exclusion criteria
The exclusion criteria was to exclude articles not to be used
in the result, because they did not meet with criteria used
in research (Polit & Beck, 2012). The criteria for each
article excluded were those that were not written in English,
those that were not relevant to nurses' experience in calling
for RRTs, articles relating to the medical rather than nursing
area, and literature reviews about RRTs. Other excluded articles
were in report form and were not complete articles, while
other articles were more than ten years old.
Table 2: Searches in PubMed
Data Analysis
Data analysis is an organisation and synthesis for
a study (Polit & Beck, 2012). All 15 articles were read
several times and then analysed. Each article was analysed
separately and independently. The main findings were highlighted
in different colours and documented on a separate piece of
paper divided into two columns. The words describing nurse
experiences were highlighted in green and words relating to
challenges were highlighted in orange. This documentation
was written up using Microsoft Word under titles and a sub
title (Curtis, 2008). All of the articles were then evaluated
in order to check their validity and reliability by looking
at the qualifications of the authors and the study design
and process (Background, Aim, Method, Results, Discussion,
Ethical Considerations, and References), the number of participants
in each study and the environment. Then each article was graded
and classified using the guidelines for the quality of an
academic article. The grade scale used was: high (I), moderate
(II), or low (III) quality (see Appendix II).
Classification of Included Articles
The quality of each article and the types of methods used
were classified based on the criteria of Berg, Dencker, and
Skärsäter (1999) and Willman, Stoltz, and Bahtsevani
(2006), and modified by Sophiahemmet University (see Appendix
II). All the results relating to the article were collected
and were written into the matrix table (see Appendix I). Each
article used different methods ranging between qualitative
and quantitative methods. Some articles used interviews or
focus groups, some used descriptive correlational design,
some used qualitative ethnographic methods, and some provided
quantitative numerical data examining the implementation of
RRTs. Of the 15 articles used, there were 10 articles that
scored grade I and the remaining articles were grade II. In
addition, all articles were appraised according to the qualifications
of each researcher and whether there were any ethical considerations
noted, aiming to determine whether the research had received
support from any company, advertisement or commercial purpose.
All the articles were checked to see whether the researcher
considered the environment of the study when collecting the
data. Furthermore, the author checked to see if the topic
was appropriate to the aim of the study. (Polit & Beck,
2012).
Ethical Considerations
Permission to do this study was obtained from Sophiahemmet
University for thesis project of a bachelor degree. The author
dealt with each study using equitably all articles being read
and using all the results in this study, and used trustworthy
data collection, analysis and interpretation to avoid any
desired finding. Paraphrasing was done after the analysis
of all articles. There was no adding of any personal information
or comments to the articles, in the strictest effort to avoid
plagiarism, falsification and fabrication while conducting
data analysis. Each study was conducted in an ethical way
during data collection and interpretation. References for
each article have been stated in order to make it easy for
the reader to locate the necessary information (Polit &
Beck, 2012).
Results
The findings in this study were based on 15 articles. These
articles focussed on nurses' experiences and challenges in
calling RRTs. The results are presented in accordance with
the research questions.
Nurses Describe Their
Experiences of Calling RRTs
Nurses' Experiences and Qualifications
Most medical-surgical nurses were familiar with calling
an RRT as part of improving patient care. Calling RRTs has
increased nurses' experiences of preparedness. However, other
medical-surgical nurses had been hesitant to call RRTs because
the physician discouraged them to call. The decision to call
an RRT depended on the years of experience of ward nurses
when there was a critically ill patient requiring intervention
from an RRT. Nurses who had 0-5 years of experience were less
likely to call an RRT, while nurses with 11 years or more
of experience called RRTs without asking other nurses (charge
nurse) or the primary team. (Salamonson, Van-Heere, Everett,
& Davidson, 2006)
The qualifications of nurses relate
to their experiences when calling an RRT for an urgent case;
those with an associate's degree in nursing (AND; who study
nursing for two years) with less than or equal to three years
of experience called at the request of another nurse (i.e.
the nurse in charge) or a physician. Comparing this response
to that of staff nurses with a bachelor of science in nursing
(BSN), who have more than three years of experience and who
study nursing for four years; they called the RRT following
the criteria provided (Pussateri, Prior, & Kiely, 2011).
Some experienced ward nurses independently
called for a RRT without waiting for any decision from the
other nurses or physicians. The decision whether or not to
call a RRT was based on the nurses' judgment on whether immediate
assistance was needed. Some bedside nurses, who often ask
for advice and consult with other nurses when unsure about
whether or not to call a RRT, were encouraged to trust their
own judgment before calling RRTs, in order to get the support
and the affirmation that they needed (Wynn, Engelke, &
Swanson, 2009).
Medical-surgical nurses perform a
synergetic role when they receive support during a call for
RRTs, where the bedside nurse brought the patient information
to the situation. The RN in a RRT team provides the knowledge
and the skills for the consultation to medical surgical nurse,
and achieves role synergy characterised by RN-RN consultation
where what is achieved from interaction is greater than that
achieved from the individual efforts. The role of synergy
between RNs is to prevent adverse events from occurring during
the rescuing process. A synergic role is an effective and
an educational tool for both nurses and patient that supports
junior and new graduate nurses, and to have the full picture
about a patient who needs support and intervention. (Leach,
Mayo, O'Rourke, 2010).
According to Wehbe-Janek et al.,(2012)
simulation experiences for bedside nurses have been used to
increase their awareness of cases when a patient needs help.
A high fidelity simulator with realistic settings was used
to identify valuable components for the nurse. The simulation
program showed the relationship of the RRT associated with
the patient outcomes. An increased familiarity with the equipment
successfully increased their effective communication skills
and gave them a sense of familiarity with the role along with
its responsibility. Debriefing and reflective learning was
used, and suggested a key future for such simulations for
effective learning.
In medical-surgical nurses' experiences,
the decision to call an RRT when they became worried for their
patient was related to self-confidence. They would increase
their awareness of the patient's condition in order to decide
whether intervention from the RRT was needed (Jones et al.,
2006).
Feelings experienced when calling
an RRT differed from one nurse to another. Bedside nurses
sometimes experienced a positive interaction with the RRT
during the call, but while some of the nurses had positive
views, others did not. A few nurses indicated that they felt
afraid when they received criticism from an RRT after calling
them. However, some nurses indicated that RRT calls were required
because the medical management by doctors had been inadequate;
many ascribed this to junior doctors and a lack of knowledge
and experience. Some bedside nurses indicated that they would
call the RRT if they were unable to call the covering doctor;
however, a minority of medical-surgical nurses preferred to
call the doctor if there was a critically ill patient before
calling an RRT. (Williams, Newman, Jones, 2011).
According to Jones et al (2006) the
majority of ward nurses indicated that calling RRTs prevents
cardiac arrest, and 97 per cent said that the RRT intervention
was intended to help and manage an unwell patient. On the
other hand, a few nurses restricted their RRT calls because
they were afraid of criticism about their patient care.
Nurses' views concerning the benefits
of calling RRTs
According to Wynn et al. (2009), there were three main reasons
to call RRTs from the bedside nurses' point of view. Around
78 per cent of the nurses surveyed (n=75) indicated that the
primary reason they call a RRT is when there is a sudden change
in the patient's vital signs. The second reason, indicated
by 56 per cent of respondents, was when there was a steady
decline in the patient's condition. The third reason, 35 per
cent, was that no adequate response had come from the physician's
side.
Some studies have shown that in most
nurses' view, in their experiences, RRT helps critically ill
patients when they have any early signs of deterioration (Astroth
et al., 2013; Leach et al , 2013; Benin et al., 2012; Bagshaw
et al., 2010).
An RRT promotes the assessment and treatment by providing
a high level of knowledge and experience, as well as helping
the nurse to prevent calling code blue to their medical-surgical
ward. An RRT also transfers an ICU level of care to the patient
in order to secure their safety. The participating nurses,
from their own experiences, believed that RRTs could prevent
critically ill patients from having a cardiac or respiratory
arrest, and that they could prevent minor issues from becoming
major and potentially life-threatening problems (Astroth et
al., 2013).
Nurses thought that RRTs could help
patients who were deteriorating fast, and cited this as the
greatest advantage of RRTs. The participants described the
RRT as a pair of eyes to assess the situation (Williams et
al., 2011).
Bedside nurses receive immediate
assistance and help for any patient in a life-threatening
situation, with early intervention for critically ill patients
to prevent cardiac or respiratory arrest. Furthermore, RRTs
provide backup support for ward nurses when they are concerned
or dissatisfied with their current medical management, or
when the ward doctor is unavailable. This backup system gives
them peace of mind in a clinical setting, and a sense of security
in knowing that there is always a backup, providing the ward
nurse with access to a medical expert who knows how to manage
emergency situations (Salamonson et al, 2006).
The majority of medical-surgical
nurse participants reported that they call the RRT if there
is a complex medical-surgical issue. They also believed that
calling the RRT would help to prevent a critically ill patient
from having cardiac and respiratory arrest. A few nurses believed
that they call the RRT because nurses have inadequate management
(Bagshaw et al., 2010).
Knowledge and Skills of Bedside
Nurses
A medical-surgical nurse identified that the RRT is a supportive
team that provides guidance, education and continued follow-up
for the patient's condition. None of the nurses noticed any
discouragement from this team during calls. Furthermore, the
unit culture of teamwork and the willingness to care for each
other's patients during an RRT event gave them confidence,
knowing that they would receive the needed assistance (Astroth
et al., 2012).
The help from RRT and the improved
skills through working as a team was immediately available
through a single phone call for nurses, who were able to obtain
additional help without having to request permission. The
RRTs were the facilities' method of redistributing the workload
for nurses (Astroth et al., 2012; Benin et al., 2012).
The support provided in calls to
RRTs from medical-surgical nurses enhanced their skills and
increased their knowledge and awareness in the processes of
nursing when they had critically ill patients. This especially
benefitted new graduate nurses, allowing them to learn from
the role of the RRTs. Some new nurses believed that calling
the RRT represented a positive and collaborative experience
that reinforces the use of teamwork. Patients also benefit
from this team when intervention occurs quickly, and as some
nurses noted, it helps them to practice their skills every
day (Williams et al., 2010).
According to Wehbe-Janek et al. (2012),
the simulation-training programme enhanced nurses' knowledge
and skills relating to medical emergency situations. An RRT
allowed them to identify their weaknesses and to learn from
their mistakes or lack of knowledge, particularly in regards
to the uncomfortable issues that they have to become familiar
with during some proper procedures, such as using an algorithm
and a crash cart. Other nurses felt that sharing ideas and
tasks expedited the assessment process and ultimately improved
the patient's condition at a faster rate.
Bedside nurses were satisfied with
the collaboration with the RN RRTs, and noted that the outcome
of the RRTs was often an improvement in skills and experiences.
However, bedside nurses also wanted to be engaged with the
team in order to provide better care for their patients, especially
when the RRT call was over and they had to care for the patient
remaining in the unit. Nurses noted that the RRTs brought
about a greater sense of appreciation for the nurses after
an RRT call, where some family members of a patient made positive
comments about their support and how they helped to save lives.
The opinion of the nurses in this study proved that they valued
RRTs, and demonstrated the positive effects that the RRTs
bring to their everyday practice. The implied positive effect
is support and empowerment for nurses (Williams et al., 2010).
Some participants amongst medical-surgical
nurses found that understanding the criteria for calling the
RRT and knowledge were important to meet the patients' needs
and to identify unstable patients. Education is important
in providing skills that will help patients (Brown, Anderson,
Hill, 2012).
Nurses' familiarity with using
the criteria for calling the RRT
When a bedside nurse calls the RRT for a critically ill patient,
he or she uses the criteria for calling the RRT based on his
or her knowledge. Critical knowledge experiences are important
in managing the crisis, and this is based on nurses' experiences
(Galhotra et al., 2006).
According to Leach & Mayo (2013)
medical-surgical nurses described that familiarity with the
team leads to trusting behaviour between them when there is
an urgent case.
The majority of participants expressed
familiarity with the RRT criteria. Around 90 per cent of nurses
thought that the RRT programme improved patient care, and
around 84 per cent felt that the service improved the nursing
work environment. Nurses who had called an RRT on more than
one occasion were more likely to value their ability to do
this (Pusateri et al., 2011).
The other nurses expressed that in their experience, the RRTs
improved their practice, since they are supported by the RRTs
when they know the criteria. Furthermore, they stated that
they receive encouragement from the nursing leader and other
co-workers. Participants in this study noted that they felt
confident when they called an RRT. Medical-surgical nurses
indicated that they received their education about RRTs during
their annual competency review. A few noted that they did
not receive any education on the RRT, other than when the
RRT was developed. Participants believed that newly graduated
nurses needed to be educated about RRTs in order to gain more
awareness about when they should call this team and for what
reasons (Astroth et al., 2012).
Communication Skills for Calling
an RRT
Nurses enhance their communication skills as another valuable
component of simulation training. Several participants described
the RRT members' communication skills as being professional
and caring. Both bedside nurses and the RRT members used the
communication tool SBAR to collect information during the
event, since this tool provides information both quickly and
accurately. The participants noted that many of the RRT nurses
provided emotional support. Others commented that they provide
encouragement to bedside nurses, and use humour to defuse
a tense situation. (Astroth et al., 2012).
In the case of an inadequately experienced
bedside nurse, he or she is required to call the RRT in an
emergency case, whereas other nurses would call the physician
first when they have a sick patient. It was noted that 55.9
per cent from the total of 351 participants that they would
call the RRT even if they were worried about any changes in
the vital signs, in order to increase their knowledge through
interaction with the RRT (Jones et al., 2006).
Common Challenges for
Nurses When Calling RRTs
Knowledge and Experiences
A lack of knowledge and experience can lead to a lack of confidence
and feelings of discomfort. Being faced with a need to exercise
judgment and decide whether or not to call the RRT is a challenge
for some bedside nurses when a medical-surgical nurse has
noticed that a patient meets the criteria for calling an RRT.
Furthermore, a lack of knowledge will lead to low quality
of patient care (Schmid, Hoffman, Wolf, Happ, & Devita,
2013).
A few medical-surgical nurses were
reluctant to call an RRT for fear of criticism from the RRT
team when they responded to the call. (Jones et al 2006)
Conflict Between the Bedside Nurse
and the Rapid Response Team
Working as a team is a major part of delivering good care
to a patient and saving patients' lives. However, in the case
of a conflict between the primary team and the nurses, or
between the primary team and the RRTs, the bedside nurses
attending felt that their plans for the patients were disrupted,
resulting in disjointed care for the patient. This is a challenge
concerning which team the bedside nurse will follow. As another
study shows, these challenges are listed under the following
two categories: direct challenge, when it is difficult to
know when to call the RRT or not, and indirect challenge,
when the RRT has been called and the question is who should
take care of the patient during the RRT's call out (Shapiro
et al., 2010).
Level of Education
Professionals who are to join RRTs need more education, training
and understanding about the philosophy behind RRTs. Other
challenges include the attitudes of RRT staff when they respond
to calls from the bedside nurses. One nurse participant noticed
that their individual's voice and communication style had
a frustrated tone, which was not encouraging during the call
out (Salamonson et al., 2006).
Traditional hierarchies and their
relation to the physicians and supervisors impede some of
the components of RN decision-making during rescue (Leach
et al., 2010).
Other nurse participants identified
that they were worried about calling RRTs because they felt
afraid of criticism from them. Other nurses feared calling
RRTs without the knowledge of the responsible nurses and physicians;
nurses observed the reaction of the team, and this made them
reluctant to call the RRT the next time. Other nurses described
situations where they wanted to call RRTs, but were reluctant
that they would be perceived as having neglected to give care
to patients (Astroth et al., 2012).
Three different studies found that
communication was a challenge when calling RRT members who
did not exhibit a communication style that the nurses perceived
as being supportive. According to the participants, their
body language and method of questioning were perceived as
negative and condescending. Moreover, their tone of voice
was not encouraging to the bedside nurse. Furthermore, the
lack of knowledge regarding the institution's policy on calling
RRTs added a confusing barrier, making the nurse reluctant
to make the call (Astroth et al., 2012; Jones et al., 2006;
Baldwin et al., 2006).
According to Bagshaw et al. (2010)
and Wehbe-Janek et al. (2012), there are other challenges
facing nurses who want to call RRTs: they become frustrated
with the delay in care when physicians are not present to
assess their patients, and they have to resist calling the
RRTs. Unavailability of assistance from co-workers created
a demand for nurses to work around the clock, losing precious
time when they should be providing care for their patient.
Some nurses identified enhanced communication as another value
of simulation training, since they were unaware of clear communication
procedures. The lack of confidence and comfort flowed in the
simulation where feelings were concerned.
Many nurses indicated that they would
not call an RRT without calling a physician first, and some
nurses feared that some doctors would shout at them when they
called the RRT. 84 per cent disagreed or strongly disagreed
that using an RRT system would increase their workload when
caring for their patients. The poor attitude from some RRTs
seems to require more education in order to deliver good communication
between the team and the staff member who is taking care of
the patient (Salamonson et al., 2006).
Discussion
Method
The literature review method was used in this study to compile
and summarise findings; each article was read and critiqued
separately and critically appraised starting with the title,
year of publication, and abstract. Next, the whole article
was analysed, including the background, aim, sampling method,
data collection, data analysis, results, discussion and ethical
approval. References were also checked for validity, credibility
and reliability. The classification of each article was assigned
following the guidelines of the quality grade (see Appendix
II). This helped the author to choose the articles that best
supported the aim. Most articles were grade I and the rest
were grade II. Graded I articles included clear abstracts
and clear processes of research, while grade II articles were
less clear in some respects.
Ethical principles were used in the
search process, including honesty, copyright for publication
and avoiding any plagiarism or misconduct such as falsification
and fabrication.
Some difficulties were faced when
searching for articles in the PubMed database. Some articles
provided more information but their year of publication was
more than 10 years ago; other articles would not open. MeSh
terms were used to find more articles relating to the topic
and to address the aim of the study. The 15 articles represented
research in different countries, but most focussed on US hospitals,
while a few were conducted in Australia.
Other challenges during the time
of this study included a lack of search results from the MeSh
database; consequently, the free search in PubMed was used.
All articles were published between the years 2005 and 2013.
Some of the articles were randomised controlled trials (RCTs),
whereas others were qualitative and prospective studies. (Poilt
& Beck, 2012).
Results
This review looked at nurses' experiences and the challenges
that medical-surgical nurses face when they call an RRT for
an urgent patient case. During the analysis of all 15 articles,
the results were categorised under the headings of 'experiences'
and 'challenges'. All of these articles addressed the research
questions and explored bedside nurses' experiences when calling
RRTs. They found that the RRT is a helpful system for patients,
and that bedside nurses felt supported by RRTs. However, there
were some challenges that needed to be overcome in order to
have a successful team delivering a good quality of care to
the patient from the points of view of both medical-surgical
nurses and the RRTs.
The themes of level of experience
and qualifications largely reflected what the nurses experienced
when calling RRTs. The findings emphasise that RRTs are an
effective tool for patient care that saves patients' lives
by preventing medical error and other adverse events (Winters
et al., 2006; Brindley et al., 2007). However, there are many
factors that can affect the performance of the system, including
human error, poor communication, and deficiency in leadership,
all of which could apply to the nursing team or the RRT (Raynard,
Reynolds, & Stevenson, 2009).
The nurses' experiences with decision-making
in trying to give quick and helpful intervention for patients
focussed on the RRT for urgent and critical cases. Nurses
are faced with the need to make a decision that requires years
of experience combined with a high level of education. Nurses
at the baccalaureate level with more than five years of experience
had self-initiated calls to an RRT for urgent cases. Thus,
education and experience are important when it comes to independent
calling. Nurses who have more experience tend to have expertise
in recognising and interpreting a situation, and are therefore
better able to manage it. All hospitals have the responsibility
to educate all healthcare professionals in order to improve
the outcome for each patient. It is important to educate nurses
about the RRT system, especially when it comes to new graduates
(Wynn et al., 2009). Feelings of worry were major reasons
for a bedside nurse to call the RRT, along with degree of
empowerment and independent action by the nursing staff. Nurses
need to know when and how to call an RRT in serious situations
(White, Pichert, Bledsoe, Irwin, & Entman, 2005; Santiano
et al., 2009).
Nurses' experiences when activating
the RRT protocol differed according to their use of the RRT
criteria, different levels of education and diverse experiences.
Some hospitals have their own protocol for calling the RRT,
and this may be different from one hospital to another (Moldenhaure
et al., 2009; Santiano et al., 2009). Decisions to call the
RRT for critically ill patients by the bedside nurse are based
on knowledge and the skills that come with years of experience
and satisfaction with RRTs. This helps them to identify the
best decision and when to call the RRT, but their qualifications
also play a role in this (Metcalf et al., 2008).
Medical-surgical nurses stated that
RRTs provide important assistance when the early signs of
deterioration are identified in order to prevent an adverse
event so as to save patients' lives. RRTs also create a teamwork
situation that generates communication among professionals,
and this communication becomes more effective when a bedside
nurse uses SBAR when reporting on the arrival of other team
members (Beebe, Brinkley, & Kelley, 2012).
Poor communication between a bedside nurse and the RRT leads
to an improper response. This indicates that poor communication
is a barrier to engaging in effective action when a patient
is critically ill, and that it is necessary to enhance nurse-physician
communication to ensure that when a nurse calls an RRT, the
response is appropriate. (White et al., 2005).
Medical-surgical nurses did not believe
that RRTs are overused in hospitals, and other participants
believed that interaction with the RRT did not increase their
workload or decrease their skills when they gave care to a
patient, but rather provided an opportunity for education
(Jolly, Bendyk, Holaday, Lombardozzi, & Harmon, 2007).
It was also considered that RRTs increase the knowledge of
the bedside nurses indirectly through the following of simulation
training, enhancing skills and awareness preparedness for
emergency team events. This was amplified by the strong response
that nurses have a better understanding of the roles of the
RRT following training (Potter & Perry, 2008). RNs in
RRTs have a synergetic role when it comes to both patients
and bedside nurses. The American Association for Critical
Care Nursing developed the synergy model, which defines some
common characteristics for patients and nurses. (Hardin,Kaplow,2005)
The patient characteristics are vulnerability,
stability, complexity and predictability. Keeping these in
mind, the nurse will be able to provide the best care according
to patients' needs. In terms of vulnerability, nurses look
for actual and potential stressors, whether physiological
or psychological, which might affect patient outcomes. Highly
vulnerable patients are susceptible to further deterioration
and poor outcomes. Stability involves maintaining a steady
equilibrium and assessing this characteristic means evaluating
a patient's ability to respond to the treatment. Meanwhile,
complexity involves the interaction of two or more systems,
and is found when patients are treated for complicated diagnoses.
Here, the nurse will assess patients for their response to
treatment and other unknown factors. Predictability is important
when it comes to nurses' identification of a predictable path
based on the disease progress and potential complications.
Here, the nurse must synthesise patient data with disease
management guidelines to ensure favourable outcomes.
The nurse characteristics are clinical
judgment, advocacy and moral agency, caring practice and collaboration.
Clinical judgment is clinical reasoning which includes decision
making, critical thinking and the global grasp of a situation
according to experiential knowledge and evidence-based guidelines.
When registered nurses are not part of an RRT, this team educates
bedside nurses' in relation to their clinical judgment through
physical and data assessment techniques that are anticipated
to be helpful for the patient. Such tools are useful for critical
care nurses when they are unfamiliar with these techniques.
In terms of advocacy and moral agency, a nurse will demonstrate
moral agency by working on the behalf and representing the
concerns of the patient. As an advocate, the RRT nurse will
be able to direct patient-centred care and ensure that patients'
wishes, dignity and rights are preserved. Moreover, in this
way, the team will provide support to patients and family
by offering clear information about the patient's condition.
The RRT also helps bedside nurses to promote decision-making.
The team acts as a conduit to exchange information amongst
the nurse, family and patient. Collaboration involves working
with others such as physicians, families and healthcare providers
in a way that promotes and encourages effective care. Each
team must respect the other teams and the role they play in
ensuring that their patient has a positive outcome (Hardin
& Kaplow, 2005).
The implementation of the RRT in
a hospital to save patients' lives distributes the work across
a team of bedside nurses, physicians and RRT members. The
RRT increases the sense of security among medical-surgical
nurses when managing an unwell patient and this may translate
into more confidence and empowerment for the nurse (Jolly
et al., 2007).
Some bedside nurses noted that they
learn new skills from interactions with RRTs, while some observed
that they want to have a special programme concerning the
RRT in order to understand when to make a call (Brown et al.,
2012). Team communication and information sharing is a critical
part of team behaviour; the Joint Commission report indicated
that communication failure is a root cause of essential events
(The Joint Commission, 2007). Communication is thus important
in delivering good care. The following three main factors
are associated with communication failure: (i) Physicians
and nurses are trained to communicate differently; (ii) the
hierarchies within the health care systems frequently inhibit
people from speaking up; and (iii) the communication and the
providers in health care (Leonard, Graham, & Bonacum,
2004).
Medical-surgical nurses and physicians
need to work as a team and accept each other's ideas. Teamwork
results in the delivery of good care to patients, as the patient
is the main concern for nurses, physicians and the RRT. Some
nurses stated that when faced with a patient who meets the
criteria for an RRT, they should call a responsible physician
before calling the RRT itself. This result suggests that the
nurse would prefer to use diplomacy instead of calling the
RRT. However, if there were no physician available, the participants
indicated that they would call the RRT (DeVita et al., 2006).
Some physicians believe that the
RRTs interfere with their plans, and this finding suggests
that more education for both nurses and physicians is needed
regarding the role of RRTs (Jolly et al., 2007). On the other
hand, delays in quick intervention relating to the lack of
a clear understanding about roles of RRTs have been a problem
when it comes to taking responsibility for whether or not
an RRT should be called. It has been suggested that simulation
training clarifies this role and increases awareness and preparedness
(Villamaria et al., 2008).
Education and teaching for bedside
nurses will improve their skills when it comes to calling
the RRT for their patients without the feeling of criticism.
More extensive education is needed in order to remove the
feeling of hesitation in calling the RRT (Pustateri, Prior,
& Kiely, 2011).
Conclusion
Medical-surgical nurses call RRTs
to help save patients' lives, and their decisions depend on
their prior experience. Medical-surgical nurses and RRTs need
to collaborate during the delivery of care to patients. Both
need to have knowledge and good communication skills in order
to identify the deteriorating clinical signs that require
intervention and to deliver fast intervention to a critically
ill patient.
The experiences of bedside nurses
who have become familiar with the signs of a deteriorating
patient and who know the criteria for calling RRT play a major
role. Years of experience and levels of qualification are
crucial in a nurse's decision to call the RRTs or to refrain
from doing so. Furthermore, the communication and attitude
of the bedside nurse and the RRT member play a large role
in delivering clear information. Finally, the patient needs
help and protection from any adverse event which could occur
while receiving care in hospital. An RRT is a helpful tool
for hospitals to apply, and can be used to educate staff.
When a patient stays in the hospital because of a medical
error, this team is needed.
Clinical Implications
The author found that, when employing RRTs in a hospital setting,
it is important to focus on educating new staff alongside
all nurses and physicians who have prior experiences with
RRTs. They should be given strategies on what their role will
be when they are faced with the need for emergency care. Education
about RRTs is important in order to avoid miscommunication
and misunderstanding between the staff that take care of patients'
wellbeing.
Recommendations for Further Studies
The author found that more studies regarding medical-surgical
nurses' perspectives on education are required in order to
address the challenges facing new staff when they call RRTs
to save their patient's life. Additional studies should also
focus on the area of improving communication among the members
of the medical-surgical team and on communication attitudes.
Click here for
Appendix 1
Click here for Appendix
2
References
Alqahtani, S., Aldorzi, H., Alknawy, B., Arabi, Y., Fong,
L., Hussain, H., et al. (2013). Impact of an intensivist-led
multidisciplinary extended rapid
response team on hospital-wide cardiopulmonary arrests and
mortality. Society of Critical Care Medicine, DOI:10.1097.
Abella, B. S., Alvarado, J. P., Myklebust, H., Edelson,
D. P., Barry, A., O'Hearn, N., Vanden Hoek, T. L., & Becker,
L. B. (2005). Quality of cardiopulmonary resuscitation during
in-hospital cardiac arrest. Journal of the American Medical
Association, 293(3), 305-310.
American Nurse Association (2011). Code of ethics for nurses
with interpretive statements. Retrieved October 21, 2013 from
http://www.nursingworld.org/Mobile/Code-of-Ethics/provision-4.html
Astroth, K., Woith, W., Stapleton, S., Degitz, R., & Jenkins,
S. (2012). Qualitative exploration of nurses' decision to
activate rapid response teams. Journal of Clinical Nursing,
22, 2876-2882.
Aveyard, H. (2010). Doing a literature review in health and
social care: A practical guide (2nd ed.). Maidenhead: Open
University Press.
Azzopardi, P., Kinney, S., Moulden, A., & Tibballs, J.
(2011). Attitudes and barriers to a medical emergency team
system at a tertiary paediatric hospital. Resuscitation, 82(2),167-176.
Bagshaw, S. M., Mondor, E. E., Scouten, C., Montgomery, C.,
Slater-MacLean, L., Jones, D. A., et al. (2010). A survey
of nurses' beliefs about the medical emergency team system
in a Canadian tertiary hospital. American Journal of Critical
Care, 19(1), 74-83.
Bellomo, R., Goldsmith, D., Uchino, S., Buckmaster, J., Hart,
G., Opdam, H., et al. (2004). Prospective controlled trial
of effect of medical emergency team on postoperative morbidity
and mortality rates. Critical Care Medicine, 32(4), 916-921.
Benin, A.L., Brogstrom, C. P., Jenq, G.Y., Roumanis, S. A.,
& Horwitz, L. (2012).
Defining impact of a rapid response team: Qualitative study
with nurses, physicians and hospital administrators. British
Medical Journal, 21, 391-398.
Berg, A., Dencker, K., & Skarsater, I. (1999). Evidensbaserad
omvardnad:Vid behandling av prisoner med depressinssiukdomar
(Evidensbaserad Omvarn, 1999:3). Stockholm, Sweden: SBU, SFF.
Brindley P,G., et al., (2007). Best clinical evidence feature.
Medical Emergency Teams: Is there M.E.R.I.T? Canadian Journal
of Anaesthesia, 54(5), 389-91.
Brown, S., Anderson, M., & Hill, P. (2012). Rapid response
team in a rural hospital. Clinical Nurse Specialities, 26,
95-102.
Beebe, P., Brinkley, K., & Kelley, C. (2012). Observed
and self-perceived teamwork in a rapid response team. Journal
for Nurses in Staff Development, 4, 191-197.
Buist, M. D., Moore, G. E., Bernard, S. A., Waxman, B. P.,
Anderson, J. N., & Nguyen, T.V. (2002). Effects of a medical
emergency team on reduction of incidence of and mortality
from unexpected cardiac arrests in hospital: Preliminary study.
British Medical Journal, 324(7334), 387-390.
Buntner, S,C. (2011). Rapid response team effectiveness. Dimensions
of Critical Care nursing , 30(4), 201-205.
Burkhardt, M., & Nathaniel, A., (2008). Ethics issues
in contemporary nursing. (3rd ed.). York: Delmar.
Chamberlain, B., & Donley, K., (2009). Patient outcomes
using a rapid response team. Clinical Nurse Specialist, 23(1),
11-12.
Cretikos, M., Parr, M., Hillman, K., Bishop, G., Brown, D.,
Daffurn, K., et al. (2006). Guidelines for the uniform reporting
of data for medical emergency teams. Resuscitation, 68(1),
11-25
Coughlan, M., Cronin, P., & Ryan, F. (2013). Doing a literature
review in nursing, health and social care. London, UK: SAGE.
Curtis, R, J. (2008). Caring for patients with critical illness
and their families: The value of the integrated clinical team.
Respiratory Care, 53(4), 480-487.
Chan, P. S., Jain, R., Nallmothu, B. K., Berg, R. A., Sasson,
C., (2010). Rapid Response Teams: A systematic review and
meta-analysis. Arcb Intern Med, 170(1), 18-26.
Dacey, J., Mirza, R., Wilcox, V., Doherty, M., Mello, J.,
Boyer, A., Gates, J., Brothers, T., & Baute, R. (2007).
The effect of a rapid response team on major clinical outcome
measures in a community hospital. Critical Care Medicine,
35(9), 2076-2082.
DeVita, M., Bellomo, R., Hillman, K., Kellum, J., Rotondi,
A., Teres, D., et al . (2006). Finding of the first consensus
conference on medical emergency team. Critical Care Medicine,
34(9), 2463-78.
DeVita, M., Hillman, K., & Bellemo, R. (2011). Rapid response
system concept and implementation. New York, NY: Springer.
Donaldson, N., Shapiro, S., & Scott, M. (2009). Leading
successful rapid response team: A multisite implementation
evaluation. Journal of Nursing Administration, 39(4), 176-181.
Dwyer, T., Mosel, W. L. (2002). Nurses' behaviour regarding
CPR and the theories of reasoned action and planned behaviour.
Resuscitation, 52(1), 85-90.
Galhotra, S., Scholle, C. C., Dew, M. A., Mininni, N. C.,
Clermont, G., & DeVita, M. A. (2006). Medical emergency
teams: A strategy for improving patient care and nursing work
environments. Journal of Advanced Nursing, 55(2), 180-7.
Geoffrey, L., Parast, L., Rapoport, L., Wagner, T. (2010).
Introduction of a rapid response system at a United States
veterans affairs hospital reduced cardiac arrest. Anaesthesia
and Analgesia, 111(3), 679-686.
Green, A., & Allison, W. (2006). Staff experiences of
an early warning indicator for unstable patients in Australia.
Nursing Critical Care, 11(3), 118-27.
Hijazi M, M., Sinno, M., & Alansar, M., (2012). The Rapid
Response Team reduces the number of cardiopulmonary arrests
and hospital mortality. Emergency Medicine, doi.org/10.4172/2165-7548.1000128.
Hardin,S.P., & Kaplow,R. (2005). Synergy for clinical
excellence: The AACN synergy model for patient care. Sudbury,
MA:Jones And Bartlett.
Hatler, C., Mast, D., Bedker, D., Johnson, R., Corderell,
J., Torres, J., et al. (2009). Implementing a rapid response
team to decrease emergencies outside the ICU: One hospital's
experience. Medical Surgical Nursing, 18(2), 84-90, 126.
Hillman, K., Chen, J., Cretikos, M., Bellomo, R., Brown, D.,
Doig, G., et al. (2005). Introduction of the medical emergency
team (MET) system: A cluster-randomized controlled trial.
Lancet, 365, 2091-2097.
Institute for Clinical System Improvement. (2013). Healthcare
protocol rapid response team. Retrieved October 16, 2013 from
https://www.icsi.org/_asset/8snj28/RRT.pdf.
Institute of Healthcare Improvement. (2001). Protecting 5
million lives from harm. Retrieved September 16, 2013 from
http://www.ihi.org/offerings/Initiatives/PastStrategicInitiatives/5MillionLivesCampaign
/Pages/default.aspx.
Institute for Healthcare Improvement. (2010). Heading off
medical crises at Baptist Memorial Hospital. Retrieved October
22, 2013 from http://www.ihi.org/knowledge/Pages/ImprovementStories/RapidResponseTeamsHeadingOffMedical
CrisesatBaptist MemorialHospitalinMemphis.aspx
Institute of Healthcare Improvement. (2013a). SBAR technique
for communication: A situational briefing model. Retrieved
September 16, 2013 from http://www.ihi.org/knowledge/Pages/Tools/SBARTechniqueforCommunicaton
AituationalBriefingModel.aspx.
Institute of Healthcare Improvement. (2013b). Vision, mission,
and values. Retrieved September 20, 2013 from http://www.ihi.org/about/Pages/IHIVisionandValues.aspx
Institute of Health Care Improvement.
(2011). Establish criteria for activating the rapid response
team. Retrieved September 20, 2013 from http://www.ihi.org/knowledge/Pages/Changes/EstablishCriteriaforActivating
theRapidResponseTeam.aspx.
International Council of Nurses. (2012). Code of ethics. Retrieved
September 16, 2013 from http://www.icn.ch/images/stories/documents/about/icncode_english.pdf.
Jenkins, S. D., & Lindsey, P. L. (2010). Clinical nurse
specialists as leaders in rapid response. Clinical Nurse Specialist,
24(1), 24-30.
Jolly, J., Bendy, K. H., Holaday, B., Lombardozzi, K.A., &
Harmon, C. (2007). Rapid response team: Do they make a difference?
Dimensions of Critical Care nursing, 26,(6) 253-60
Jones, D., Baldwin, I., McIntyre, T., Story, D., Mercer, I.,
Miglic, A., et al. (2006). Nurses' attitudes to a medical
emergency team service in a teaching hospital. Quality and
Safety in Health Care. 15(6), 427-32.
Keller, S., Edstrom, A., Parker, W., Gabriele, C., & Kriewald,
M. (2012). Scope and standard of medical surgical nursing
(5th ed.): Academy of Medical Surgical Nurses.
Kemper, K., Bulla, S., Krueger, D., Ott, M. J., McCool, J.
A., & Gardiner, P. (2011). Nurses' experiences, expectations,
and preferences for mind-body practices to reduce stress.
BMC Complementary and Alternative Medicine, 11, 1-9.
Konrad, D., Jäderling, G., Bell, M., Granath,F., Ekbom,
A., Martling, C. (2009). Reducing in-hospital cardiac arrests
and hospital mortality by introducing a medical emergency
team. Intensive Care Medicine. 36(1), 100-6.
Leach, L., Mayo, A., & O'Rourke (2010). How RNs rescue
patients: A qualitative study of RNs' perceived involvement
in rapid response teams. British Medical Journal, 19, 13.
Leonard,M., Graham, S., & Bonacum, D. (2004). The human
factor: The critical importance of effective teamwork and
communication in providing safe care. Quality Safe in Health
Care, 13(1), 85-90.
Leach,L.S.,& Mayo,A.M.(2013). Rapid response team: qualitative
analysis of their effectiveness. American Journal of Critical
Care,22:198-210.
Metcalf, R., Scott, S., Ridgway, M., Gibson, D., et al. (2008).
Rapid response team approach to staff satisfaction. Orthopaedic
nursing, 27(5), 266-71.
Clinical triggers: An alternative to a rapid response team.
Joint Commission Journal on Quality and Patient Safety, 35(3),
164-74.
Wynn, J., Engelke, M., Swanson, M. (2009). The front line
of patient safety: Staff nurses and rapid response team calls.
Quality Management in Health Care, 18(1), 40-47.
Moldenhaure, K., Sabel, A., Chu, E. S., & Mehller, P.
S. (2009). Clinical triggers: An alternative to a rapid response
team. Joint Commission Journal on Quality and Patient Safety,
35(3), 164-74.
National Council of State Boards of Nursing. (2013). Nurse
practice act, rules & regulations. Retrieved October 20,
2013 from https://www.ncsbn.org/1455.htm.
National Patient Safety Agency (2007). Safe care for the acutely
ill patient: learning from serious incidents. London: NPSA.
National Confidential Enquiry into Patient Out Come And Death.
(2005). An acute problem? A report of the national confidential
enquiry into patient out come and death. London: NCEPOD.
Peberdy, M. A., Kaye, W., Ornato, J. P., Larkin, G. L., Nadkarni,
V., Mancini, M. E., et al. (2003). Cardiopulmonary resuscitation
of adults in the hospital: A report of 14,720 cardiac arrests.
The National Registry of Cardiopulmonary Resuscitation, 58(3),
297-308.
Polit, D. F., & Beck, C. T. (2012). Nursing research:
Generating and assessing evidence for nursing practice (8th
ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Potter, P. A., & Perry, A. G. (2008). Fundamentals of
nursing. (7th ed.) Maryland Heights, MO: Mosby Elsevier.
Pusateri, M. E., Prior, M. M., & Kiely, S. C. (2011) The
role of the non-ICU staff nurse on a medical emergency team:
Perceptions and understanding. American Journal of Nursing,
111(5), 22-29.
Ray, E. M., Smith, R., Massie, S., Erickson, J., Hanson, C.,
Harris, B., & Willis, T. S., (2009). Family alert: Implementing
direct family activation of a pediatric rapid response team.
Joint Commission Journal on Quality and Patient Safety, 35(11),
575-580.
Rogers, A., Hwang, Ting Hwang, S., Aiken, L., & Dinges,
D. F. (2004). The working hours of hospital staff nurses and
patient safety. Health Affairs, 23(4), 202-212.
Santiano, N., Young, L., Hillman, K., Parr, M., Javasinghe,
S., & Baramy, L. S. (2009). Analysis of medical emergency
team calls comparing subjective to objective call criteria.
Resuscitation, 80(1), 44-49.
Salamonson, Y., Heere, B., Everett, B., & Davidson, P.
(2006). Voices from the floor: Nurses' perception of the medical
emergency team. Intensive And Critical Care Nursing, 22, 138-143.
Shapiro, S., Donaldson, N., & Scott, M., (2010). Rapid
response teams seen through the eyes of the nurse. American
Journal of Nursing, 110(6),28-34.
Sharek, P. J., Parast, L. M., Leong, K., Coombs, J., Earnest,
K., Sullivan, J., Frankel, L.P, & Roth, S. J. (2007).
Effect of rapid response team on hospital-wide mortality and
code rates outside the ICU in a children's hospital. Journal
of the American Medical Association, 298(19), 2267-2274.
Scott, S., & Elliott, S. (2009). Implementation of a rapid
response team: Success story. Critical Care Nurse, 29 (3),66-75.
Schmid, M., Hoffman, L.A., Wolf, G. A., Happ, M. B., &
DeVita, M. A. (2013). The use of medical emergency teams in
medical and surgical patient: Impact of patient, nurse, and
organisation characteristics. Quality Safe in Health Care,
17, 377-381.
The Joint Commission. (2007). National Patient Safety Goal.
Oakbrook Terrace, IL: The Joint Commission: 2007.
Thomas, K., Force, M., Rasmussen, D., Dodd, D., & Whildin,
S. (2007). Rapid response team, challenges, solutions, benefits.
Critical Care Nurse, 27(1), 20-27.
Villamaria, F., Pliego, F., Wehbe-Janke, H., Coker, N., Rajab,
H., et al. (2008). Using simulation to orient code blue team
to a new hospital facility. Simulation in health care, 3(4),
209-216.
Wehbe-Janke, H., Lenzmerire, Carissa., Ogden, P., Pat Lambden,
M.,Sanford, P., et al. (2011). Nurses' perception of simulation-based
interprofessional training program for rapid response and
code blue event. Journal of Nursing Care Quality, 27(1), 43-50.
White, A., Pichert, J. W., Bledsoe, S, R., Irwin, C., &
Entman, S. S. (2005). Cause and effect analysis of closed
claims in obstetrics and gynecology. Obestetric Gynecolog,
105(5), 1031-1038.
Williams, D. J., Newman, A., Jones, C., Woodard, B., (2011).
Nurses' perceptions of how rapid response teams affect the
nurse, team, and system. Journal of Nursing Care Quality,
26(3), 265-72.
Willman, A., Stoltz, P., & Bahtsevani, C. (2006). Evidensbaserad
omvårdnad: En bro mellan forskning och klinisk verksamhet
(2:a uppl.). Lund: Studentlitteratur.
Winter, B. D., Pham, J. C., Hunt, E. A., Guallar, E., Berenholtz,
S., & Pronovost, P,J. (2007). Rapid response team: A systematic
review. Critical Care Medicine, 35, 1238-1243.
Winters, B.D., Pham, J., Pronovost, P. (2006). Rapid Response
Team: Walk, don't run. The Journal of The American Medical
Association, 296(13), 1645-7.
Vincent, C. (2010) Patient safety (2nd ed.). Chichester: Wiley-Blackwell.
Young, L., Donald, M., Parr, M., & Hillman, K. (2008).
The medical emergency team system: A two-hospital comparison.
Resuscitation, 77, 180-188.
|
 |




