| |
February
2014
- Volume 8, Issue 1
Nurse-led chest
drain clinic: a case study of change from national health
system in UK

|
 ( (
|
Abdulsalam
Y Taha (1)
Akeel S Yousr (2)
Kamil J Zaidan (3)
(1) Prof. Abdulsalam Y
Taha, Department Of Thoracic And Cardiovascular Surgery,
School Of Medicine, University Of Sulaimania And Sulaimania
Teaching Hospital, Sulaimania, Region Of Kurdistan,
Iraq. E MAIL: salamyt_1963@hotmail.com PHONE: 009647701510420
(2) Dr. Akeel S Yousr, Department Of Thoracic And Cardiovascular
Surgery, Ibn-Alnafis Teaching Hospital For Thoracic
And Cardiovascular Surgery, Baghdad, Iraq.
(3) Dr. Kamil J. Zaidan, Kadimia Teaching Hospital,
Baghdad, Iraq.
Correspondence:
Prof. Abdulsalam Y Taha,
Head of Department of Thoracic and Cardiovascular Surgery,
School of Medicine, University of Sulaimania, Sulaimania,
Region of Kurdistan, Iraq
PO Box: 414.
Phone: 009647701510420
Email: salamyt_1963@hotmail.com
|
 |
|
Abstract
Background and Objective: There are many nurse-led
clinics now in the UK, such as Chest-Pain, Endoscopy
and Bronchiectasis Clinics. Herein, we present the project
of Nurse-led Chest Drain Clinic in Guy's and St Thomas,
s Hospital, London. The aim is to analyze this change
project.
Methods: A project of change was designed to
set up an outpatient clinic run by specialist clinical
nurses for patients discharged home with an ambulatory
chest drain system in situ. The project is observed
and analyzed via interviews with the responsible nurses.
Results: The clinic was established in 2005 and
run by two Nurse Case Managers. 60 patients were seen
in 2007 and the clinic remained well attended. Patients
were happy to spend less time in hospital as they could
stay safely with their families.
Conclusions: A safe at home management of long-term
chest drains was provided by this nurse-led clinic.
Key words: chest drain, nurses, outpatient clinic
|
Introduction
The National Health System in the United Kingdom (UK) has
witnessed dramatic changes in the role of nurses over the
last 2 decades. The professional standard of nurses has very
much improved. The public has realized this change and their
trust in services provided by nurses has also increased. There
are many clinics now in the UK run by specialized nurses such
as Chest-Pain Clinic, Endoscopy Clinic, Bronchiectasis Clinic
and others.[1,2] Thoracic surgery is no exception. Patients
with chest drains placed for different indications like drainage
of air and/or fluid in the pleural space are usually managed
in hospital till the drainage stops and the chest tube is
removed. This sometimes necessitates a long stay in hospital
for persistent air and/or fluid drainage. This is undoubtedly
associated with increased cost and burden on hospital resources.
More time should be spent by physicians looking after such
patients until they can be discharged home with no chest drain.
Herein, we present the project of Nurse-led Chest Drain Clinic
in Guy's and St Thomas's Hospital, London. The aim is to analyze
the process of successful change achieved by nurses in this
project.
Materials and Methods
A project of change was designed to set up an outpatient clinic
run by clinical nurse specialists for patients discharged
home with an ambulatory chest drain system in situ. The project
is observed and analyzed via interviews with the responsible
nurses. Place: the clinic was located at Guy's Hospital in
the Cardiothoracic Outpatient Department, 1st Floor, Thomas
Guy's House.
Clinic Times: Monday afternoon 14.00 to 16.00, 4 slots
of 30 minutes per patient.
It was run by 2 Nurse Case Managers; both had specialized
thoracic surgery skills and experience.
Patient Population: any patient with a chest drain
in situ who can be managed at home by a District Nurse, or
patients who had recently had a chest drain in hospital and
required follow up.
On discharge home, the patient was given an information sheet
and his/her District Nurse was informed by phone about the
care of chest drain at home. The first appointment would be
after 1 week. The nurse would assess level of fluid output
and/or history of air leak. A chest X-ray would be ordered
and reviewed by the clinic nurse specialist with the consultant
thoracic surgeon or registrar. A clinical decision was to
be made as to remove or keep the drain. Chest drain would
be removed by the nurse when necessary. The consultant's message
was clear: whenever in doubt, do not remove the chest drain.
A letter would be written to the GP, thoracic surgeon or the
oncologist. A weekly follow up was necessary as long as the
drain remained in situ.[3] Most patients with air leak could
have their chest drain removed in 2 weeks. Examples of the
devices used in patient's care are shown in Figures 1-3. The
community nurses used to be afraid of caring for a patient
with a chest drain. This fear was alleviated by annual workshops
held in the department to educate them about chest drain care
and other health topics.
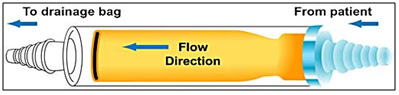
Figure 1: Heimlich chest drain valve
Source: www.medicine-on-line.com
image 011

Figure 2: Heimlich valve attached to chest tube
Source: www.vygonvet.co.uk

Figure 3: a plastic bag attached to chest drain.
Source: The Guy's and St Thomas, NHS Foundation Trust December-2007
Newsletter
Results
The change took about 6 months. The clinic was established
with co-operation of the consultant surgeons and other stakeholders.
The actual work in the clinic began in 2005. An audit of all
patients visiting the clinic was kept by the Nurse Case Manager
on Excel. Numbers and outcomes were recorded. During the year
2007, 60 patients were seen i.e., 5 patients per week. "The
Chest Drain Clinic remains well-attended, we see an increase
in the number of patients managing their long-term drains
at home and we are happy for patients to spend less time in
hospital when they prefer to be at home closer to their families"[4]
said the nurse case managers. Patients and their relatives
felt happier, being earlier discharged and staying at home.
Discussion
The Thoracic surgical department in Guy's Hospital at the
time of the study had 4 consultant thoracic surgeons, 2 senior
nurses and 28 beds.[3] The number of beds was considered relatively
small in relation to the size of the served population (estimated
to be around 15 million persons).[3,4] It is well known that
patients with persistent air leak and/or fluid drainage may
occupy beds for a long time thus putting a burden on hospital
resources. The few surgeons in the department used to spend
a considerable time in the follow up of such patients.
The idea of shifting the care of patients with chest drains
after leaving the hospital, from doctors to nurses, was thus
born for many reasons. The Guy's and St Thomas, NHS Foundation
Trust encouraged projects which aimed at a better use of beds,
providing enough beds for cancer patients which comprised
75% of thoracic surgery work in Guy's Hospital [3] and shortens
the waiting period before operations and thus meeting the
national guidelines for cancer therapy.[3] Better use of beds
and money saving is expected from such a project without affecting
the patient's care. There were 2 senior nurses who specialized
in thoracic surgery working in the department. They used to
look after patients with chest drains while they were in the
ward. They strongly believed that they could do the same service
in an outpatient clinic. Although no Chest Drain Clinic was
run before in UK, there were similar nurse-led projects in
NHS like chest pain and endoscopy clinics which stimulated
the Thoracic Surgery Specialist nurses to go ahead in their
project. Literature review included a few similar models in
other countries which formed a background for the project.[5]
The literature also demonstrated that outpatient management
of patients with spontaneous pneumothorax or even prolonged
air leak appeared safe, efficient and economic.[6] The nurse
specialists were further encouraged by the co-operation and
support of the consultant surgeons. Patients always preferred
to be at home as opposed to being in the hospital. The public
in UK are increasingly aware about the current roles played
by nurses in NHS. The communication system between the Senior
Case Managers, patients and Community Nurses was good enough
to support the new project beside the recent availability
of compact, self-contained, clean and more user-friendly devices
which can be strapped to the belt have been provided by manufacturing
companies. [6] Therefore there was little to worry about.
On the other hand, the nurse case managers embarking on this
change realized some potential threats to their success like
slippage of the drain after patient's discharge, inability
of the District Nurse to look after the chest drain, the clinic
might not be considered a real clinic as that run by doctors
and a minority of patients may prefer to be seen by the consultant
rather than the nurse case manager.
The skilled nurse case managers shared a future vision with
the doctors and agreed upon establishing the new clinic. They
had put a plan forward that consists of identification and
addressing the stakeholders as well as changing the systems
of discharge, follow-up and referral of patients.
The identified stakeholders were: doctors (consultant surgeons
and oncologists, GPs and juniors), patients, hospital manager,
manufacturing companies and public. All were supportive; however,
junior doctors did not make proper referrals initially.
In conclusion, out-patient care offered by nurse-led clinics
to patients with chest drain for prolonged air leak provided
many advantages over the in-patient care. The successful implementation
of the change project highlights the techniques necessary
to achieve similar changes.
References
1. Sharples L. A randomized control crossover trial of nurse
practitioner versus doctor led outpatient care in a bronchiectasis
clinic. Thorax 2002;57:661-6.
2. Moore S. Nurse led follow up and conventional follow up
in management of patients with Lung Cancer. BMJ 2002;325:1145-8.
3. The Guy's and St Thomas, NHS Foundation Trust December-2007
Newsletter.
4. The Guy's and St Thomas, NHS Foundation Trust December-2008
Newsletter.
5. Robert James Cerfolio. Closed Drainage and Drainage Systems.
In: G. Alexander Patterson et al, editors. Pearson's Thoracic
& Esophageal Surgery, Vol 1. 3rd ed. Philadelphia: Churchill
Livingstone Elsevier; 2008.p.
6. Myatt R. An exploration of the patient experience following
discharge from hospital with a long term chest drain (unpublished
MSc dissertation). Imperial College, London University. 2005
|
 |




