| |
February
2014
- Volume 8, Issue 1
A holistic
approach to bedside teaching from the views of main users

|
 ((2) ((2)
|
Leili Mosalanejad
(1)
Mohsen Hojjat (2)
Morteza Gholami (3)
(1) Assistant professor,
Mental health Department, Jahrom University of Medical
Sciences, Jahrom, Iran
(2) Nursing PhD student, Nursing Department, Jahrom
University of Medical Sciences, Jahrom, Iran
(3) English instructor, Jahrom University of Medical
Sciences, Jahrom, Iran
Correspondence:
Leila Mosalanejad
Assistant professor, Mental health Department,
Jahrom University of Medical Sciences, Jahrom, Iran
Phone: 0791-3341508
Mobile: 09177920813
Email: mossla_1@yahoo.com
|
 |
|
Abstract
Introduction: Clinical education concerns with
acquiring lots of skills and competencies that enable
health professionals to function properly and provide
services effectively. The aim of this study was to evaluate
a holistic examination on bedside teaching from the
views of its main users.
Materials and methods: This is a cross sectional
study on 70 teachers (clinical and nursing), 70 students
(medical and nursing), 400 patients in Jahrom University
of Medical Sciences. Data gathering tool was a three-part
questionnaire in which the first part was assigned to
demographic data, the second part was 10 five-part questions
aiming at investigating bedside teaching quality for
teachers, students, and patients. Reliability was 0.83,
0.78, and 0.89 respectively.
Results: The results showed that teachers evaluated
bedside teaching in three areas of communication skills
(50.4), proper clinical examination (44.4), and developing
professional skills (44.4) more than other fields. Sharing
some in common, the students also had a higher average
in acquisition of professional skills (83.3) enhancing
knowledge of students (82.3) and obtaining a suitable
model of communication (72.3). The patients also considered
factors such as high self-esteem, feeling of satisfaction
(3.83), humanized health care (3.83), and transfer of
information to both teachers and students (3.83) higher
than other factors.
Conclusion: According to the results, it is necessary
to appropriately train teachers to meet these standards,
and while justifying students to implement this method
and its benefits, patients' satisfaction, enhancing
health care, and effective clinical governance should
be provided.
Keywords: Bedside teaching, Teachers, Students,
Effectiveness
|
Introduction
Bedside teaching includes any kind of training in the presence
of the patient, regardless of the environment in which this
training is presented. Several studies indicated that clinical
teaching is an effective method of training and today it is
used less than in the past, but students, patients, and faculty
members strongly support this teaching method(Subha and 2003).
In this way, clinical skills related to communication between
doctor and patient, physical examination, clinical reasoning
and obtaining specific skills of professionals will be learned
better than classroom instruction methods (Williams, et al.
2008). Ramani and colleagues also expressed the benefits of
clinical teaching as communication skills, clinical examination
findings, teaching human aspects of clinical medicine and
creating conditions to model professional behavior, so that
these qualities cannot be shown effectively in the classroom
(Ramani, et al. 2003).
Furthermore, the clinical teaching provides opportunities
for teachers to observe students (EI-Bagir and Ahmed 2002)(4).
There is also evidence that suggests that these patients also
enjoy this teaching method, because they gain a better understanding
of the disease (Janick and Fletcher 2003)(5). In research
conducted by Williams Kit and colleagues on four-year medical
students and internal residents in first and second years
in medicine school at Boston University, students believed
that clinical teaching is valuable and necessary to learn
clinical skills and expressed that this method is used less
frequently and there are many obstacles in performing it,
including lack of respect to the patient, time constraints,
lack of attitude, knowledge and skills of the teachers, and
also mentioned strategies for solving these problems(Williams,
et al. 2008) (2).
Ramani and colleagues conducted a study focused on four groups
including senior assistants, skilled teachers in clinical
teaching, faculty members of hospitals affiliated to Boston
University and named the main obstacles as reduction of clinical
teaching skills, and the fear of clinical teaching. They believed
that teachers should be trained in almost all unreachable
levels of clinical diagnosis and this puts them under a lot
of pressure. They expressed that teaching is less important
than research in the universities and teaching ethics is missing.
Thus, they presented some strategies to eradicate these obstacles
including: developing clinical teaching skills by teaching
faculty members in clinical skills and teaching methods, ensuring
that teachers possess great capabilities in clinical teaching,
making a learning atmosphere to allow the teachers to accept
their limitations, and eliminate low value of teaching in
the departments with appropriate recognition and considering
rewards for the successful teachers. In the present study,
expert teachers and professors stated that the ethics of clinical
teaching must be established on emphasizing the importance
of using this method to get students to think clinically(Ramani,
et al. 2003).
Aldeen and Gisondi also conducted a study on clinical teaching
in emergency department and expressed that the emergency department
is an ideal atmosphere for clinical teaching because of high
volume of patients, high acuity and severity of diseases and
pathologies that provide a variety of patient-centered educational
opportunities(Aldeen and Gisondi 2006).
One of the major concerns of the clinical teachers is creating
a learning-teaching approach to transfer learning which occurs
in the teaching environment to the real and clinical environment.
Since interaction between medical staff and patients is considered
as an important fact in clinical work and is necessary for
treatment process and this interaction is in the presence
of the patient, therefore, research and teaching strategies
should be as close as possible to the real environment (Brien
2002). Clinical training mission is to train qualified students
with necessary knowledge, attitudes, and skills, and to achieve
this objective, standardized clinical training is an essential
component of the educational programs, since approximately
50% of the teaching programs are dedicated to clinical works
(Irma, et al. 2011). It is generally accepted that research
methods should focus on beliefs, values, and behavior of teachers
in the education system (Karimi Moonaghi et al 2010). But
in recent years, research on teaching methods and their applications
are more superficial and thus, deeper investigation is required
(Heimlich and Norland 2002) . Clinical teaching is a valuable
method used by teachers despite their relative familiarity
with it. Another notable point is failure to meet teaching
standards in implementing this method and lack of appropriate
use of it in clinical teaching. The aim of this study is to
investigate quality and effectiveness of bedside teaching
on students, teachers, and patients' points of views and determine
constraints and challenges and propose strategies to remove
them and finally, positive steps are taken to use these teaching
methods more effectively.
Materials and Methodologies
This is a cross-sectional study to investigate the effectiveness
of bedside teaching on teachers, medical students, and patients'
attitudes in the hospital affiliated to Jahrom University
of Medical Sciences. Cluster random sampling was carried out
on medical students in various fields of medical sciences
(medical and nursing students) and all nursing and clinical
faculty. Approximate number of students in the two groups
of medicine in three levels (externs - Interns) and nursing
and training courses were 70. 50 teachers of different groups
(nursing and medicine) participated in this study that performed
clinical teaching for the students. In the patients' group,
in a two-month period, all patients who were present in bedside
teaching numbered 400 and bedside teaching was carried out
on them.
Approving the research proposal and obtaining approval of
the research director, validity of the questionnaire was confirmed
according to reliable sources (1, 3, 6), and then 10 expert
professors confirmed it. Reliability in three sectors (teachers
- students and patients) was proved with Cronbach's alpha
by working on a pilot sample respectively (0.78- 0.83 and
then 0.89). The questionnaires were given to students (doctors,
nurses), patients and staff and then coded, collected, and
analyzed using SPSS statistical software. It is worth mentioning
that the questionnaires were designed by Likert method (never,
to very high, 0-4) and in addition to demographic questions,
11 more questions were included which assess the effectiveness
of clinical teaching from the viewpoints of masters, students,
and patients. Data was analyzed using descriptive statistics
such as mean, standard deviation, and Spearman and K2 test.
Inclusion criteria for the study were the interest of students,
teachers and patients to participate in the study, as well
as internship and performing bedside teaching by the teachers
and exclusion criteria included illiterate patients, patients
with somatic and psychiatric disability, patients in critical
units because of the lack of accountability, patients where
this method was not determined in their wards and patients
in ambulatory wards.
Results
The results showed that the pattern of acquisition of good
communication, training, performing physical exam, gaining
professional skills and increased general information have
a higher average. From the students' views, gaining professional
skills and increasing students' general information and obtaining
appropriate communicative plans have higher average.
Table 1: Mean score of bedside
teaching quality from the perspective of both teachers and
students
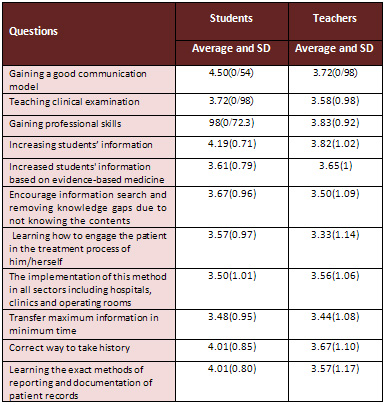
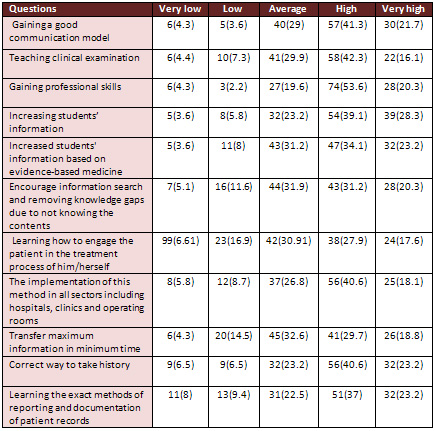
Table 2 shows that most students considered the quality of
bedside teaching from moderate to high.
Table 2: Descriptive statistics
of the effectiveness of bedside teaching from students' views
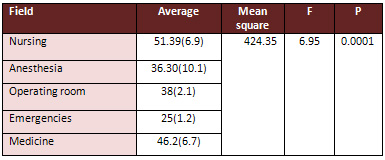
Additional
results showed that there is a significant relationship between
the effectiveness of bedside teaching and field of study (02/0
P = ,60/17 X2). But there is no relationship between age,
sex, and method effectiveness. There is a significant relationship
between viewpoints of both sexes on the effectiveness of bedside
teaching (T= 3/87, P= 0.02). Other results showed that there
is a significant difference among students in terms of fields
of study.
Table 3: Mean differences in terms of effectiveness of
bedside teaching based on field of study
Additional results related to the
effectiveness of this method indicated that the majority of
patients were in the age groups 60-51 years (25.3%) and the
majority with 43.3% in wards, 52% men's internal ward, and
48% women's ward, and majority had primary education.
Table 4 shows that this method is most effective in raising
self-esteem and feelings of patient satisfaction and cause
medical care to become humanistic and useful information passes
to students and the teachers.
Table 4: Mean of effectiveness
on bedside teaching from the patients' views
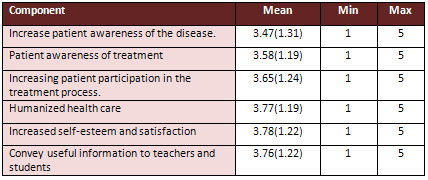
59.9% of the patients evaluated the bedside teaching as high
and very high, 26.5% average, and only 3.3% low and very low.
Other results showed that the quality and effectiveness of
this method are high, and very high from the viewpoints of
patients. Other results showed that there is a significant
relationship between age and education in terms of correlation
between age and effectiveness of bedside teaching (p= 0.008,
r= 0.15).
But there is no significant relationship between the effectiveness
of bedside teaching in terms of sex, kind of disease, the
ward, and the education.
Other results indicated that there is a significant relationship
between patients' viewpoints of effectiveness of bedside teaching
based on age (F=2.47, P=0.03). But as other cases show, it
is suggested that the effectiveness of the method based on
demographic variables was not significant.
Table 5: Difference of bedside
teaching effectiveness based on demographic variables

Discussion
The results show that obtaining a good communicative pattern,
appropriate teaching, clinical examination, acquisition of
professional skills and increasing students' scientific information
on the viewpoints of teachers have a higher average.
In another study conducted to investigate the experiences
of advisor faculties and fourth-year students of medicine
in a qualitative study on bedside teaching of medical students
and advisor faculties, advisor faculties were under pressure
considering time spent over other commitments, despite enjoying
this approach. The results showed that all of the teaching
strategies used by the teachers were not welcomed with great
enthusiasm by the students. Students considered the teachers
as an educational model (Stark 2003a).
In a study conducted by Celenza, Rogers, with the aim of investigating
the effectiveness of bedside teaching on patient care with
a 6-month perspective study in emergency department, people
stated that the most common lesson they took from this method
was skills in history taking and physical examination and
cited clinical reasoning as the most important lessons learned
from this approach(Celenza and Rogers 2006).
Studies conducted by Gonzalo et al on 51 local residents and
102 medical students from educational rounds and bedside teaching
revealed that time spent in clinical practice for the learners
to learn bedside teaching is very important for professional
development and that this method is preferred by the learners
compared with other methods of bedside teaching training (Gonzalo,
et al. 2009).
In another study, hospitalists spent an average of 101 minutes
on teaching rounds and an average of 17 minutes inside patient
rooms or 17% of their teaching time at the bedside. This study
showed rounds that included time spent at the bedside were
longer on average than rounds that did not include time spent
at the bedside(Crumlish, et al. 2009).
In research conducted on 27 patient attendants, 22 patients,
and 21 residents, the attendants expressed their satisfaction
with bedside teaching and presented a case report in a conference
room in a linear range. 96 versus 92 out of 100 linear parts,
expressed their preferences with bedside teaching (95 vs.
15), and comfort (89 vs. 19) in this range. But there was
no significant difference in residents' satisfaction and comfort
in applying this method. These people were more comfortable
in asking questions (84 vs. 69), having the art of asking
questions (85 vs. 67) in the conference room. This study showed
that 81% of patients' attendants wished that the next examination
was with their patient.
Evidence shows that bedside teaching includes 61% of clinical
training and performed examinations. This method takes more
time than the typical round (Landry, et al. 2007).
A study conducted to evaluate this educational method and
its impacts on the attitudes of students and patients, revealed
that although there is a slight difference among some students,
to present the contents away from the patient's bedside, students
expressed that students learned more about diagnosing and
staying by the patients' bedside at the time of bedside teaching.
But students' knowledge of mechanism of diseases was lower
than presentation out of clinical wards(Rogers, et al. 2003).
In a study conducted on 108 patients and 142 fourth-year medical
students at Washington University, students and patients preferred
bedside teaching as a teaching method; patients more easily
communicate with doctors and talked about their health issues.
Also, two groups of patients and
students benefited more from participating in bedside teaching
(17).
In another study aiming at examining viewpoints of internal
residents and medical students, it became clear that this
approach is effective in developing skills such as history
taking 55%, physical examination skills (89%) professional
72%, physician-patient communication skills 83%, differential
diagnosis 43%, and patients' management 59% (Jed, et al. 2009).
Some evidence states that outcome of this method is dependent
on 1) the value of peer assessment in a group , (2) variety
of teaching strategies, (3) the opportunities to provide feedback
to learners, (4) the art of asking questions effectively,
and (5) the possible relationship between a teacher's skills
and successful bedside teaching (Beckman 2004).
In another study the importance of peer assessment was investigated
and the benefits such as high value of using peer assessment,
applying an unlimited number of teaching strategies, applying
this method to revive missed opportunities, the art of asking
question effectively, and the relationship of teacher maturity
and bedside teaching were emphasized. The results of this
study are the same with the abovementioned results considering
bedside teaching approach so that the development of communication
skills, performing proper clinical examination, and improvement
of professional skills, were expressed as the most important
results regarding the quality of this method.
The results also showed that all of the teaching strategies
used by teachers in this method may not be welcomed by the
students. And, despite the fact that students and teachers
are partners in education, general agreement about the quality,
quantity and clinical teaching may fail to be materialized
considering appropriate clinical teaching(Stark 2003b).
In the present study, despite acceptable reported quality
of bedside teaching and its clinical aspects (moderate to
high) which indicates the relative familiarity and acceptable
application of this educational method, lack of time is considered
as an obstacle to applying this technique.
The positive effects of this method can be noted as numerous
roles of the clinical teachers including, actor, director,
audience, passive, and listener. Also, in presenting this
method, the patients undergo less passive roles and mere audience
(Lynn 2009). This can justify the obtained results regarding
patients' satisfaction and their consent to participate in
this educational method.
Also, the positive effects of this method on patients' participation
in health care plans and changing their positions due to participation
can be noted as an advantage of this method. However, no negative
impact on patients' care was found. The results of this study
are consistent with the results presented in the following
study (Celenza and Rogers 2006).
Other advantages of this method may include opportunities
to gather additional information, direct observation of learners'
performance, humanizing care for patients, non-judgmental
language, improving patients understanding of their disease
and feeling active on the side of patient(Janicik and Fletcher
203). All of these outcomes justify patient satisfaction with
the use of this method.
Given the quality of the bedside teaching provided by main
users of this educational method, it is necessary to consider
different approaches and strategies such as clinical skills,
teaching methodologies by the teachers, ensuring the application
of this method aiming at understanding these points to rely
on their knowledge and skills, creating a learning environment
that allows teachers to become aware of their limitations
and examine their capabilities, sufficient reward for the
efforts of the teachers, and emphasis on the revival of ethics
in bedside teaching (Ramani, et al. 2003).
Among other strategies to reduce barriers examining the clinical
setting, are addressing time constraints by adopting a flexible
training program, proper patient selection, ensuring the learners,
improve learner autonomy in the teaching process, and developing
evidence-based education. (Keith, et al. 2008).
Conclusion
Considering the importance of bedside teaching method and
regarding the good views of the teachers, patients, and middle
and high students' views, it is necessary to provide training
classes to develop teachers' capabilities, justify the students
and mention its benefits, and to pave the way to use this
method appropriately. Also, using this method considering
the positive and appropriate patients' views, can provide
a holistic analysis of health care and improve health and
to provide effective implementation of clinical governance.
Acknowledgement:
This study is the result of a research plan approved by Jahrom
University of Medical Sciences. Hereby we would like to express
sincere gratitude to the research assistant of the university
for financial support.
References
1. Subha R. Twelve tips to improve bedside teaching. Medical
Teacher, ,2003 ;25( 2): 112 - 115.
2. Williams K, Rammani S, Fraser B, Orlander JD. Improving
Bedside Teaching: Findings from a Focus Group study of learners.
Acad med 2008 ; 83: 257-264.
3. Ramani S, Orlander JD, Strunin L, Barber TW. Whither bedside
teaching? A focus group study of clinical teachers. Acad med
2003; 78: 384-390.
4. EI-Bagir M, Ahmed K. What is happening to bedside clinical
teaching? Med Educ 2002; 36: 1185-1188.
5. Janicik RW, Fletcher
KE. Teaching at the bedside: a new model. Med Teach 2003;
25 (2): 127 - 130 .
6. Aldeen AZ, Gisondi
MA. Bedside Teaching in the Emergency Department. Acad Emerg
Med. 2006 Aug;13(8):860-6.
7. Brien RO. An overview
of the Methodological Approach of Action Research. 2002. Available
from: http: // www. Web.Net/~robrien/ papers/ arfinal.html
8-. Irma H. Mahone ,
Sarah P. Farrell ,Ivora Hinton , Robert Johnson ,et.al. Participatory
Action Research in Public Mental Health and school of Nursing:
Qualitative findings from an Academic - community partnership.
Journal of Participatory Medicine; 2011 ,3.
9. KarimiMoonaghi H ,Dabbaghi
F ,Oskouieseid F ,Vehvilainen-Julkunen K.I. Binaghi T Teaching
style in clinical nursing education: A qualitative study of
Iranian nursing teacher's experiences. Nurse Education in
Practice 2010; 10: 8-12.
10. Heimlich J E. , Norland E. , 2002. Teaching style: where
are we now? New Directions for adult and continuing Education
93 , 17- 25.
11. Stark P. Teaching
and learning in the clinical setting: a qualitative study
of the perceptions of students and teachers. Medical Education
2003;37(11):975-982.
12. Celenza A , Rogers
IR. Qualitative evaluation of a formal bedside clinical teaching
programme in an emergency department. Emerg Med J 2006;23:769-773
.
13. Gonzalo JD , Masters PA Simons RJ , Chuang CH. Attending
rounds and bedside case presentations: medical student and
medicine resident experiences and attitudes. Teaching and
Learning in Medicine 2009;21(2):105-10.
14. Landry MA , Lafrenaye
S , Roy MC , Claude Cyr C. A Randomized ,Controlled Trial
of Bedside Versus Conference-Room Case Presentation in a Pediatric
Intensive Care Unit. Pediatrics 2007;120;275-280
15.C rumlish C M ,Yialamas
M A ,McMahon G T. Quantification of bedside teaching by an
academic hospitalist group. Journal of Hospital Medicine 2009;4(5):
304-307.
16. Rogers HD , Carline
JD , Paauw DS. Examination room presentations in general internal
medicine clinic: patients' and students' perceptions. Acad
Med. 2003 Sep;78(9):945-9.
17. Rogers HD Carline
JD , Paauw DS. Examination room presentations in general internal
medicine clinic: patients' and students' perceptions. Acad
Med. 2003 Sep;78(9):945-9.
18. Jed D. Gonzalo ,Philip
A. Masters and Richard J. Simons, Cynthia H. Chuang. Attending
Rounds and Bedside Case Presentations: Medical Student and
Medicine Resident Experiences and Attitudes. Teach Learn Med.
2009; 21(2): 105-110.
19. Beckman T J. Lessons Learned
from A Peer Review of Bedside Teaching. Academic Medicine
2004; 79(4): 343-346.
20. Stark P. Teaching and learning
in the clinical setting: a qualitative study of the perceptions
of students and teachers. Medical Education 2003;37(11):975-982.
21. Lynn V. Monrouxe
. The Construction of Patients' Involvement in (Attewell 2006)
Hospital Bedside Teaching Encounters. Qual Health Res July
2009 ; 19 (7): 918-930.
22. Celenza A, Rogers IR. Qualitative
evaluation of a formal bedside clinical teaching programme
in an emergency department. Emerg Med J 2006;23:769-773 .
23. Janick WR ,Fletcher
KE. Teaching at the bedside: a new model. Medical Teacher
2003; 25( 2) : 127-130 .
24. Keith N W, Subha R, Bruce
F , Jay D O. Improving Bedside Teaching: Findings from a Focus
Group Study of Learners. Academic Medicine 2008 ; 83 ( 3 ):
257-264
Further
reading
Aldeen, A.Z., and M.A. Gisondi. 2006 Bedside Teaching in the
Emergency Department. 2006; by the society for academic Emergency
medicine doi: 10. 1197/J.aem. 2006. 03. 557. Acad Emerg Med
13(8):860-6.
Attewell, J. 2006 From research and development to mobile
learning: Tools for education and training providers and their
learner. The International Review of Research in Open and
Distance Learning 7(3):Available from www.irrodl.org.
Beckman, T .J. 2004 Lessons Learned from A Peer Review of
Bedside Teaching. Academic Medicine. 79(4):343-346.
Brien, R.O. 2002 An overview of the Methodological Approach
of Action Research. Available from: http: // www. Web.Net/~robrien/
papers/ arfinal.html.
Celenza, A., and I.R. Rogers 2006 Qualitative evaluation of
a formal bedside clinical teaching programme in an emergency
department. . Emerg Med J 23.:769-773
Crumlish, C. M., M. A. Yialamas, and G.T. McMahon 2009 Quantification
of bedside teaching by an academic hospitalist group. Journal
of Hospital Medicine 4(5):304-307.
EI-Bagir, M., and K. Ahmed 2002 What is happening to bedside
clinical teaching? . Med Educ 36:1185-1188.
Gonzalo, J.D., et al. 2009 Attending rounds and bedside case
presentations: medical student and medicine resident experiences
and attitudes. Teaching and Learning in Medicine 21(2):105-10.
Heimlich , J.E. , and E. Norland 2002 Teaching style: where
are we now? New Directions for adult and continuing Education
93: 17- 25.
Irma, H. M., et al. 2011 Participatory Action Research in
Public Mental Health and school of Nursing: Qualitative findings
from an Academic - community partnership. Journal of Participatory
Medicine 3.
Janicik, R.W ., and K.E. Fletcher 203 Teaching at the bedside:
a new model. Med Teach 25(2):127-130.
Janick, W.R., and K.E Fletcher. 2003 Teaching at the bedside:
a new model. . Medical Teacher 25 ( 2):127-130
Jed, D. G, et al. 2009 Attending Rounds and Bedside Case Presentations:
Medical Student and Medicine Resident Experiences and Attitudes.
Teach Learn Med. 21(2):105-110.
KarimiMoonaghi, H., et al. 2010 Teaching style in clinical
nursing education: A qualitative study of Iranian nursing
teacher's experiences. Nurse Education in Practice 10:8-12.
Keith, N.W., et al. 2008 Improving Bedside Teaching: Findings
from a Focus Group Study of Learners. Academic Medicine .
83(3):257-264.
Landry, M.A., et al. 2007 A Randomized Controlled Trial of
Bedside Versus Conference-Room Case Presentation in a Pediatric
Intensive Care Unit. Pediatrics 120:275-280.
Lynn, V. M. 2009 The Construction of Patients' Involvement
in Hospital Bedside Teaching Encounters. Qual Health Res 19(7):918-930.
Ramani, S., et al. 2003 Whither bedside teaching? A focus
group study of clinical teachers. . Acad med 78: 384-390.
Rogers, H.D., J.D. Carline, and D.S. Paauw 2003 Examination
room presentations in general internal medicine clinic: patients'
and students' perceptions. Acad Med.. 78(9):945-9.
Stark, P. 2003a Teaching and learning in the clinical setting:
a qualitative study of the perceptions of students and teachers.
Medical Education 37(11):975-982. 2003b Teaching and learning
in the clinical setting: a qualitative study of the perceptions
of students and teachers. Medical Education. 37(11):975-982.
Subha, R., 2003 Twelve tips to improve bedside teaching. Medical
Teacher 25( 2):112 - 115.
Williams, K., et al. 2008 Improving Bedside Teaching: Findings
from a Focus Group study of learners. Acad med 83:257-264.
|
 |




