| |
October
2013 - Volume 7, Issue 5
Nurses' Perceptions
of Pain Assessment and Pain Management for Patients with Myocardial
Infarction in a Coronary Care Unit

|
 ( (
|
Sharifa
Alasiry (1)
Caroline Löfvenmark (2)
(1) Sharifa Alasiry,
MSN. CCRN
(2) PhD. Lecturer, Sophiahemmet University College,
Stockholm
Correspondence:
Sharifa Alasiry, MSN.
CCRN
Email: sharifaalasiry@yahoo.com
|
 |
|
Abstract
Background: Pain is one of the most common medical
problems that occur in hospitals; in spite of its incidence,
there are many patients who suffer with untreated pain.
Unrelieved pain can negatively impact a person's quality
of life, causing activity life disturbances like psychological
distress; anxiety, depression and lack of sleep. Cardiovascular
disorder is a significant global health problem, which
accounts for the death of a third of people of the world.
Chest pain is the most common symptom of heart attacks.
However, some patients will present with pain in other
areas like pain in arm, shoulder, neck, teeth, jaw and
back pain. In literature there is little observational
research to investigate actual pain assessment and management
practices of critical care
nurses in routine clinical practice for patients with
myocardial infarction.
Aim: The aim of this study was to explore nurses'
perceptions regarding pain assessment and pain management
for patients with Myocardial Infarction in a coronary
care unit.
Methodology: The study
was a qualitative design, using semi structured interviews.
Ten critical care nurses who work in a coronary care
unit were interviewed. The author used a qualitative
content analysis approach to analyze the interviews
by doing the manual analyzing and having different themes.
Result: Three main themes were indentified in
this study and each theme had different categories which
are presented as the following: Dealing with patients
who have myocardial infarction pain is challenging;
there are different approaches in pain assessment including
subjective and the third theme is Holistic approaches
to pain management.
Conclusion: Critical
care nurses need more skills and knowledge to practice
good pain assessment and effective pain management when
they deal with patients who have myocardial infarction
pain. In this study patients who do not verbalized their
pain lack the proper assessment of pain due to inability
to communicate their pain. More research is needed in
this area of pain assessment and management especially
for patients with myocardial infarction.
Key words: Pain, Myocardial Infarction, Critical
Care Nursing, Coronary Care Unit, Perception, Pain assessment,
Pain management.
|
BACKGROUND
The experience of pain is a complex phenomenon, and it involves
social, cultural, emotional, psychological and physiological
components. Pain in critical care areas is triggered by anxiety,
fear and difficulties in communication (Adam & Osborne,
2005). It is estimated that the majority of patients in America
suffer from pain and many of those patients suffer from acute
or chronic pain during their hospitalizations (McCarberg,
Nicholson, Todd, Palmer, & Penles, 2008).
Overview of pain
Pain is one of the most common medical problems that occur
in hospitals; in spite of its incidence, there are many patients
who suffer with untreated pain (McCarberg et al., 2008). Pain
is a complex, subjective phenomenon; it means unpleasant feeling,
which results from tissue injuries. Moreover, pain induces
many harmful effects, which inhibit early recovery from critical
illness (Morton & Fontaine, 2009). According to Lindberg
& Engström (2011, P.164) the International Association
for the Study of Pain (IASP) defines pain as "an unpleasant
sensory and emotional experience associated with actual or
potential tissue damage or described in terms of such damage".
Words like "hurt, discomfort, unpleasant" are concepts
that are linked to pain (Montes-Sandoval, 1999).
It is documented in literature that
pain should be considered to be the fifth vital sign, and
to be measured and documented regularly as heart rate, blood
pressure, respiratory rate and temperature (Shannon &
Bucknall, 2003). There are three types of pain; mechanical,
thermal and chemical pain. Mechanical pain occurs when a person
has high pressure in the site of pain. Thermal pain occurs
if a person is exposed to extreme heat or cold. The chemical
pain is caused by outside agents, for example acids cause
stomach pain. Acute pain refers to limited pain duration;
usually the autonomic nervous system is activated and it responds
well to analgesia (Mann & Carr, 2006).
Pain is one of the most important stressors that patients
experience in critical care units. It works synergistically
with sleeplessness and contributes to confusion and results
in increased morbidity and mortality (Glynn & Ahern, 2000).
It is reported by physicians that pain has a negative impact
on the quality of life of persons who suffer from pain; patients
with chronic pain reported that pain had harmful effects on
their mental health, employment status, sleep, and personal
relationships (Montes-Sandoval, 1999; McCarberg et al., 2008).
Unrelieved pain can negatively impact
a person's quality of life, causing activity life disturbances
like psychological distress; anxiety, depression and lack
of sleep (Montes-Sandoval, 1999; McCarberg et al., 2008).
Shannon & Bucknall (2003) state in their study that there
are physiological complications associated with pain, including
increased pulmonary complications and increased cardiac work
as well as depression and anxiety. Pain is known to be an
important symptom to be considered for treatment in critical
care areas. It is important for nurses and physicians to do
a proper assessment and achieve adequate pain relief, because
the majority of patients in critical care units mention that
they experienced moderate to severe pain during their admission
(Gelinas, 2007). In critical care areas patients experience
different stressors, although painful memories are blurred
by different drugs but patients can still recall their pain
experience during their admissions (Morton & Fontaine,
2009).
Gate control theory of pain
According to Mann & Carr (2006) the gate control theory
of pain is described by Melzack & Wall in 1965, wherein
they used their physiological and psychological knowledge
to propose this theory. The transmission impulses from afferent
fibers to spinal cord transmission to the T-cells are modulated
by a gating mechanism. There are different fibers that influence
the gate mechanism. There are two types of fibers; small and
large fibers. Usually the large fibers try to inhibit transmission
by closing the gate while the small fibers tend to open the
gate and facilitate the transmission of impulses. The spinal
gating mechanism is influenced by nerve impulses that go down
from the brain. When the amount produced of the spinal T-cells
exceeds a critical level, it activates the action system and
the person experiences pain.
Myocardial infarction pain
Cardiovascular disorder is a significant global health problem,
which accounts for the death of one third of the people in
the world. In critical care units; the management goal for
patients with cardiac disorders is to maximize cardiac output
and reduce cardiac workload (Morton & Fontaine, 2009).
The majority of cases that are presented with heart attack
and chest pain are due to having a clot or a plaque that occludes
blood vessels. When there is an occlusion to the arteries,
it causes a block in the blood flow and when this occurs the
heart is starved of oxygen and therefore, the heart cells
die (Chen& Zieve, 2011). Chest pain is the most common
symptom of heart attacks, however, some patients will present
with pain in other areas like pain in arm, shoulder, neck,
teeth, jaw and back pain. The characteristics of heart attack
pain will be as following; heavy chest, squeezing heavy pressure
on chest, anxiety, cough, dizziness, irregular heartbeats,
shortness of breath, sweating, nausea or vomiting (Chen &
Zieve, 2011; Hwang, Ahn &Jeong, 2012).
Pathophysiology of pain in myocardial
infarction
Atherosclerosis is the narrowing or the occlusion of a coronary
artery, which may be caused by the presence of thrombus. Having
good artery blood flow is very important for the myocardium
function. The coronary arteries being open are important in
the maintenance of normal cardiac performance. Failure to
meet the demands of the myocardium of oxygen as a whole may
lead to congestive heart failure. Ischemia of certain areas
may lead to the clinical symptom of cardiac pain or disturbances
of impulse formation and conduction in the form of arrhythmias.
If the ischemia is sustained, actual injury e.g. myocardial
infarction, may develop (Blumgart & Zoll, 1960; Marieb,
2006).
Diagnosis of myocardial infarction
Different blood tests are used to diagnose myocardial infarction.
In myocardial infarction; time is very important because there
are correlations with patient symptoms, electrocardiograms
(ECG), and angiographic studies. There are different biomarkers,
which have a clear association with acute myocardial infarction
(Morton & Fontaine, 2009). The total Creatine Kinase (CK)
is a simple and inexpensive test that is available in many
hospitals. Yet, its elevation is not a specific indicator
for myocardial infarction (Medical libraries: Mercer the University
school of Medicine, 2012). Creatine Kinase MB (CK-MB) is a
more specific test for cardiac muscle. It usually increases
within three to four hours of myocardial necrosis, then peaks
in a day and returns to normal within 36 hours (Medical libraries:
Mercer the University school of Medicine, 2012). Also there
is another test and it is called Troponin; Troponin T and
I are components of cardiac muscle. They will increase if
there is myocardial injury. Troponins increase post MI within
three to 12 hours, about the same timeframe as CK-MB. Troponin
"I" remains elevated longer than CK-MB up to five
to 10 days, and up to 2 weeks for troponin "T".
Moreover, there are other blood tests that include Myoglobin,
B-type Natriuretic Peptide and C-reactive protein (Medical
libraries: Mercer the University school of Medicine, 2012).
If a patient with a heart attack is stable with normal vital
signs and consciousness, the patient can go for coronary angiography
test. And in this test, X-ray is used to see how the blood
flows through the main arteries (Adam & Osborne, 2005;
National Institute for Health and Clinical Excellence, 2010).
Management of
myocardial infarction
Pharmacological management of myocardial infarction
Emergency treatment includes close observation in the emergency
room, giving oxygen, and administering some medications like
Nitroglycerin, Morphine for vasodilatation action to relieve
pain, anti platelet and anti thrombin agents.
Relief of pain is one of the most important aspects when treating
patients with myocardial infarction. Intravenous Opioids,
for example Morphine, are the analgesic most commonly used.
Administration of aspirin and heparin reduces the incidence
of subsequent re-infarction (Van de Werf, Bax, Betriu, Blomstrom-Lundqvist
& Crea et al., 2008). Patients with MI are admitted to
critical care units especially coronary care units to receive
thrombolytic therapy and have close monitoring (National Institute
for Health and Clinical Excellence, 2010).
Non pharmacological management
of myocardial infarction
Patients with cardiac diseases develop anxiety and therefore,
the assessment of anxiety should be a part of regular nursing
care because the nursing assessment of anxiety can help patients
to adapt to the diseases and help those patients to have a
better outcome (Trotter, Gallagher & Donoghue, 2011).
The values of the holistic care which include; symptom management,
interaction with patients and their family, holistic care,
therapeutic environment, and identification of patients' needs
should be connected with nursing (Kolcaba, Tilton & Drouin,
2006). Nurses play an important role in pain management. In
critical care units nurses practice doing messaging for patients,
diversion activities and practice deep breathing. Having non-pharmacological
interventions may help in alleviating patients suffering of
pain and it increases quality of nursing care by reducing
stress and anxiety (Lindberg & Engström, 2011).
Coronary Care Units
The first coronary care unit (CCU) was developed in the mid
1960s to treat patients with myocardial infarction. Since
that time critical care nurses have expanded their roles to
take care of all cardiovascular disorders (Morton & Fontaine,
2009). There is various equipment in the CCU, including advance
machines, defibrillators, resuscitation carts and emergency
drugs (Adam & Osborne, 2005). Advanced technology influences
every aspect of critical care units and it is integral to
the assessment and monitoring of patients and the treatment.
It also helps to access vital information and enhances data
communication (Funk, 2011). Critical care areas provide care
for patients who need close observation and special treatment
that cannot be provided in general wards. Patients who are
admitted to coronary care areas need to have special care,
which is provided by well-trained personnel including critical
care nurses (Adam & Osborne, 2005).
Critical Care Nurses
Nurses in critical care areas should be competent, knowledgeable
and well trained to deal with critically ill patients (Shannon
& Bucknall, 2003). There are many challenges in a critical
care nursing unit, for instance dealing with critically ill
patients, different diagnoses, and cultural diversities among
people, multilingual staff and sophisticated technology (Morton
& Fontaine, 2009). According to St Marie (2002) Henderson
defined nursing as "the unique function of the nurse
is to assist the individual, sick or well, in the performance
of those activities contributing to health or its recovery
(or to peaceful death) that he would perform unaided if he
had the necessary strength, will or knowledge and to do this
in such a way as to help him gain independence as rapidly
as possible" (P.483).
In addition, human experience of pain occurs in different
contexts for example; physical, psycho spiritual, socio-cultural,
and environmental contexts (Kolcaba, Tilton & Drouin,
2006). Nurses in critical care units owe the duty to take
care of all patients who need help; moreover nurses have responsibility
and accountability to maintain patients' integrity and safety
when patients have pain (Morton & Fontaine, 2009).
Critical care nurses depend on teamwork with other staff in
providing optimum care for the patients in critical care units.
Physicians are required to prescribe medications, including
analgesics and sedatives, which are often utilized synergistically
to control pain in critical care units. In spite of staff
knowledge and skills development, there is documented information
of delayed recognition of patients with acute illnesses (Shannon
& Bucknall, 2003).
Collaborative work in critical care areas are documented in
the literature and this of course leads to better outcomes
for patients. Good critical care practice leads to prevent
emergency situations by applying a proper assessment and close
observation (Adam & Osborne, 2005). However, poor early
recognition and lack of skills to recognize patients with
acute illness lead to poor outcomes for patients and increases
the mortality rate (Shannon & Bucknall, 2003; Adam &
Osborne, 2005). Nurses in cardiological units play an important
role in improving quality of care. Nurses are in a unique
position to implement the correct practice in critical care
units. Moreover, bedside nurses have firsthand knowledge about
compliance to follow up patient care (Hyden &Fields, 2010).
Comfort care theory in nursing
Comfort care theory is considered as art in nursing (Kolcaba,
Tilton & Drouin, 2006). This includes a process of comforting
actions, which are performed by a nurse on a patient. According
to comfort theory, patients need comfort in stressful health
care situations; family members of those patients also need
to have comfort and support. Many patients' needs can be identified
by a nurse who then implements comfort measures to meet the
patients' needs. Providing comfort enhances healthy behaviors
and peaceful death. Using this theory of comfort helps to
release patients' suffering and distress; it also can support
the patients to experience a feeling of comfort (Kolcaba,
Tilton & Drouin, 2006).
Nurses' role in pain assessment
Different approaches have been used in hospitals to assess
pain clinically, for example self-report, behavioral-observational
methods and using different scales (Hadjistavropoulos &
Craig, 2004). Pain assessment is challenging in critical care
units (Skrobik, 2008). In any critical care unit a patient
assessment includes the following, history, physical assessment,
electro cardio gram (ECG), invasive and noninvasive monitoring,
biochemical and hematological tests, chest x-ray and other
diagnostic tests (Adam & Osborne, 2005).
Pain is one of the most common problems and stressors in any
critical care area including CCU. Therefore, nurses in critical
care areas need to have a clear meaning of the concept of
pain assessment to achieve effective pain control (Morton
& Fontaine, 2009).
Using nursing models and assessment
tools to assess pain makes nursing care a continuing process.
Assessment tools and other nursing models help to optimize
the quality of care and improve the outcome for patients who
have acute illness. If nurses can assess patients' pain correctly,
pain can be treated more effectively, and patients will report
less pain and suffering (O'Connor, 1995). A study has been
done by Valen, Vuuren, Domburg, Woerd, Hofland & Bogers
(2012), which showed that when nurses use the protocol "a
nurse-driven pain protocol" in patients with post-cardiac
surgery there was an absolute reduction in pain scores. Moreover,
the use of a nurse-driven pain protocol was safe and effective
in many cases; an evaluation of patients' safety showed no
readmission of patients to an ICU because of any factor related
to administration of pain medication (Hadjistavropoulos &
Craig, 2004; Morton & Fontaine, 2009).
There are varied circumstances present
in critical care units which interfere with pain assessment,
for example acuity of the patients' conditions, altered level
of consciousness, inability of a patient to communicate pain
and the patient's immobility (Hadjistavropoulos & Craig,
2004; Morton & Fontaine, 2009). Critical care nurses and
doctors try to obtain the patient's self report of pain and
do a good assessment; although there are different factors
that interfere with a proper assessment. The factors that
interfere with pain include the use of sedation, mechanical
ventilation and inability of patients to communicate verbally
(Ge´linas & Johnston, 2007).
There are other predisposing factors
that restrain adequate pain assessment; they include the presence
of technology and the rapidly changing situations of patients.
The factors that interfere with pain assessment are common
in critical care units and they limit nurses' ability to make
a proper decision regarding pain assessment and also implement
their decisions regarding pain management (Shannon & Bucknall,
2003; Puntillo, Smith, Arai & Stotts, 2008).
For patients who are unable to do
a self-report of pain or communicate well, nurses need to
have observable behavioral and physiologic indicators, which
are used as indicators for the assessment of pain. Furthermore;
patients who are not able to provide their self-report of
pain verbally or with other signs (e.g., head nodding, pointing
to a scale), the use of a valid behavioral pain scale is strongly
recommended (Hadjistavropoulos & Craig, 2004; Ge´linas
& Johnston, 2007; Puntillo, Smith, Arai & Stotts,
2008; Gelinas, Arbour, Michaud, Vaillant & Desjardin,
2011).
Since the 1980s there has been documentation
that pain assessment improves pain management, and decreases
patients' suffering. Yet, there is a lack of pain assessment
documentation, which indicates a gap between research and
practice. Also there is little observational research to investigate
actual pain assessment practices of critical care nurses in
routine clinical practice (Shannon & Bucknall, 2003).
Nurses' roles in pain management
The management of pain includes pharmacologic, non-pharmacologic,
or a combination of both and nurses are expected to develop
the skill of balancing those treatment options (Puntillo,
Smith, Arai & Stotts, 2008). In contemporary nursing,
early recognition of pain and proper intervention enhances
good patient outcomes, moreover; early recognition of pain
shortened hospital stay and decreased cost. Organizations
have a responsibility to ensure staff competency in pain assessment
and management because an individual has a right to have proper
pain management when needed (St Marie, 2002).
Organizations' performance is measured by ensuring patients'
satisfaction, and meeting needs and expectations (St Marie,
2002). Ethically, pain management depends on a professionals'
understanding of a patients' pain. Health care providers have
to examine and assess what forms quality of life for their
patients, especially, when a patient is in pain and with patients
with a cognitive impairment who are not able to communicate
their pain (Hadjistavropoulos & Craig, 2004).
Patients have the right to receive optimal pain relief and
to be involved in their pain management. Patient advocacy;
nurses have an obligation to explore all the options of pain
managements within the scope of nursing practice. Patients
who may not be able to communicate their pain should have
close observation and proper pain management. Liabilities
resulting from improper pain management means the failure
of adherence to good practice (St Marie, 2002).
According to Lindberg & Engström (2011), assessment
and treatment of patient's pain in postoperative care is crucial
and it is a common task for critical care nurses. Nurses'
knowledge in the field is essential because patients are looking
to receive optimal nursing care. If a patient is pain free
after a surgery, it means that comfort has increased and the
period of hospital admission is reduced (Puntillo, Smith,
Arai & Stotts, 2008).
Critical care nurses and physicians maintain themselves to
have a strong commitment to pain relief, but still there is
documented statistics of underestimation and under-treatment
of their patients' pain (Skrobik, 2008). In some studies there
are a number of barriers that avoid effective pain management
in critical care units. These barriers include inability to
communicate with patients, presence of complicated technology,
less nursing knowledge and having limited time to attend to
patients' care. Moreover, critical care nurses continually
fail to deal with these barriers and to assess patients' pain
accurately (Montes-Sandoval, 1999; Shannon & Bucknall,
2003).
Perception
Nurses deal with pain from a holistic perspective as with
other symptoms (Montes-Sandoval, 1999). Nurses' awareness,
attitudes and beliefs regarding pain have a significant impact
on the effectiveness of pain management. Therefore nurses'
roles in pain management are considered to be an important
aspect in order to evaluate the effectiveness of nursing care
(Edwards et al., 2001). National Open University of Nigeria
(2009, P.18) defines perception as "important cognitive
factors of human behavior or psychological mechanism that
enable people to understand their environment". Also
perception is defined as "the processes whereby people
select, organize, and interpret sensory stimulations into
meaningful information about their work environment"
National Open University of Nigeria (2009, P.18).
Cambridge Dictionary Organization (2012) defines perception
as "a belief or opinion often held by many people and
based on how things seem".
Also "Perception is defined as an act of being aware
of one's environment through physical sensation, which denotes
an individual's ability to understand" (Cambridge Dictionary
Organization, 2012).
In this study, perception means the
nurses' awareness, beliefs and experiences which the nurses
perceive or gain when they do pain assessment and pain management
for patients who have myocardial pain. Since perception as
a concept has different meanings in nursing this may influence
nurses' practices.
PROBLEM STATEMENTS
It has been reported that nurses underestimated the patients'
pain in half of patients who have myocardial infarction, mostly
when the patients were in severe pain (O'Connor, 1995). Nurses'
documentation of the pain assessment was inadequate with respect
to severity and duration of the patients' pain (O'Connor,
1995). There is development in nursing knowledge every year.
Despite this development there is documented data that critical
care nurses underestimate and under medicate the patients
with pain (Glynn &Ahern, 2000). Finally, good pain assessment
and pain management for patients in critical care units is
a significant factor in maximizing patients' recovery. Although,
with this proof there is little evidence in clinical practice
that critical care nurses have improved their pain assessment
and pain management practices (Shannon & Bucknall, 2003;
Skrobik, 2008). Therefore, studying nurses' perceptions, which
includes knowledge and experiences of nurses, becomes a very
important part in nursing research.
AIM
The aim of this study was to explore
nurses' perceptions regarding pain assessment and pain management
for patients with Myocardial Infarction in a coronary care
unit.
METHODOLOGY
Methods
The study was a qualitative design, using semi structured
interviews (Polit & Beck, 2008). Content analysis is a
research method that has been used in health studies and it
is a qualitative study, which includes analyzing narrative
materials (Hsieh & Shannon, 2005). Qualitative content
analysis research deals with contextual meaning of the text.
It aims to provide an understanding of given texts. It uses
the subjective interpretation of the content of text data
through the systematic classification process of coding and
identifying themes or patterns (Hsieh & Shannon, 2005).
Further, content analysis is a research method that provides
an objective means of describing data or other documents (Elo
& Kynga, 2008). It enhances understanding of the different
data especially narrative. In the content analysis, it is
possible to make the words of transcribing data condensed
by placing them in categories. Moreover in content analysis
the same data, which shares the same meaning, is classified
into the same categories. One of the purposes of content analysis
is to make a model, conceptual system or categories (Elo &
Kynga, 2008).
Participants and procedure
The participants were ten critical care nurses who have
more than one year of experience in the CCU. They used to
deal with myocardial infarction patients in the selected unit.
The author did the selection of the participants randomly
with the cooperation of the charge nurses in the chosen ward
by using the inclusion criteria. All the ten nurses met the
author and were given the written and oral information about
the study (see Appendix III). The author explained to the
participants the voluntariness and ability to withdraw from
the study anytime during the study; after that the author
met each nurse separately and explained the study aim, method
and ethical consideration. Finally, the author conducted the
interviews in different shifts with the voluntary nurses.
Inclusion criteria
The participants spoke the English language and had a diploma
or a Bachelor degree in nursing. The study included nurses
who work full time in the coronary care unit and who were
willing to participate in this study.
Data Collection
The data were collected in five days and in different shifts
"morning, evening and night time" by doing semi-structured
interviews using an interview guide. To test the credibility
of the questions; the author tested the questions by doing
two pilot interviews with two nurses who work in the same
unit, and no changes were made to the original questions since
they were clear to nurses. Both tested interviews answered
to the aim of the study, and thereby were included in the
result (Polit & Beck, 2008).
The author did ten interviews including
the two pilot interviews. Each interview lasted for 20 minutes
and was done on the coronary care unit in one hospital. The
interviews included open-ended questions to help the participants
to explain their perceptions regarding pain assessment and
pain management (Polit & Beck, 2008). Moreover, the author
asked some follow up questions during the interviews to make
questions and answers more clear (see Appendix IV). A tape
recorder was used in order to help the author in the transcription
of data. The nurses accepted to be tape recorded (Polit &
Beck, 2008). The interviews were transcribed verbatim, and
the author reviewed the transcripts to ensure accuracy of
collected data during transcription (Graneheim & Lundman,
2004).
Data Analysis
The author used a qualitative content analysis to analyze
the interviews by doing the manual analyzing, as described
by Graneheim & Lundman, (2004). Each interview was read
by the author to get a comprehension of the data. The author
read all transcribed data several times again, and all the
meaning units were identified. All the data were transcribed
verbatim and relevant information was extracted (Graneheim
& Lundman, 2004). The transcribed data was entered into
a word program in the author's computer to keep data safe
through all the process of transcriptions. Then meaning units
were written in tables followed by writing the condensed meanings
for each text. The condensed meanings were put under different
codes, which share the same meanings. The codes, which have
common meaning, were set in varied categories. The last step
of the analysis included the formation of themes (see Appendix
I). Finally the author got three main themes, which were latent
meaning (Table 2). The author used the aim of the study to
guide the analysis of data.
ETHICAL
CONSIDERATIONS
The study was done with approval
from the hospital administration and nurses' services department
(see Appendix II). Written information about the study was
given to all participants before doing the interviews. The
names of the participants were not revealed for confidentiality
issues. International council of nurses' code of ethics takes
care of the participants' information and voluntariness so
the author considered this aspect during processing the study
(International Council of Nurses, 2012). The author considered
the autonomy of the participants in answering the questions,
according to the Declaration of Helsinki; the author considers
the participants' rights to withdraw from the study or to
refuse to answer the questions for any reason (World Medical
Association [WMA], 2012). During the interviews the author
considered the privacy of the place and confidentiality of
the participants, so the interviews took place in the nurses'
sitting room in the chosen CCU as it was preferred by the
nurses. The interviewees were coded with no references to
their names. The author respected information and ideas of
the participants and during the transcription the author spoke
honestly during all the research process with no alteration
to the original data.
RESULTS
In the result there are three main themes, which refer
to nurses' perceptions regarding pain assessment and pain
management for patients who have myocardial infarction in
a coronary care unit. The demographic data of participants
are shown in Table 1.
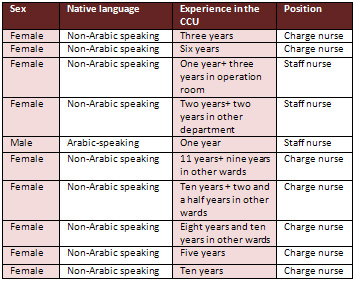
Table 1: Demographic data of the participants
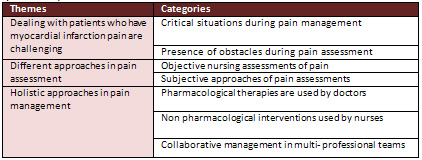
Table 2: Three main themes
and each theme has different categories
Dealing with patients who have myocardial infarction pain
is challenging
In this theme there are two categories, which the author formulates
after analyzing the data. The categories explain how nurses
find dealing with myocardial infarction cases as challenges
because there are some barriers, obstacles and difficulties,
which, may happen during pain assessment or pain management.
Critical situations during pain
management
In this category there are different situations, which are
seen by nurses as critical situations because of the presence
of emergency events or serious complications. Nurses state
if a patient develops any complication of MI like complete
heart block; emergency medications, and equipment should be
available too for rapid intervention in case of arrhythmia.
"We should keep crash cart
stand there and the defibrillator we do not know maybe a patient
get cardiac arrest any time"
Nurses verbalize other serious situations especially when
a patient has sudden deterioration at the time of discharge
from a hospital. Unexpected situations have been seen as critical
situationsin the nurse's perception. Moreover, some nurses
explain myocardial infarction diagnosis as difficult because
it is complicated and if the diagnosis is not correct the
patient might be damaged by incorrect treatment. Failing to
get the correct diagnosis is a very difficult experience for
nurses. Further, nurses in the coronary care unit perceive
management of the patient with acute MI as a challenging situation
and it needs rapid interventions and good monitoring to save
the patient's life.
"When we do ECG we get to know it is already MI, it
is complicated and it is not easy situation"
Thrombolytic therapy is one of the
most common treatments that are used to treat patients with
MI. However there are some complications of thrombolytic therapy
as nurses mentioned during pain management, including bleeding
and arrhythmia. Nurses must be aware and alert all the time
to observe the patient in case complications occur. Nurses
in the CCU perceive situations with complications are really
serious and critical.
" In thrombolytic therapy
we should be careful with a patient, we should set the patient
and observe him, sometimes there is some arrhythmia, sometimes
bleeding during the thrombolytic therapy and other complications,
so we need to observe the patient seriously plus we need to
have all emergency equipments near to the patient"
Presence of obstacles during pain
assessment
In this category there are varied factors that interfere
with pain assessment. Nurses see these factors as obstacles
that affect good assessment. Language barriers are very important
factors that are verbalized by many nurses. Another obstacle,
which happens during pain assessment, is to have non-verbalizing
patient who cannot verbalize his pain. Moreover, some patients
will not give correct, timing of onset of pain, which leads
to improper pain management.
"Because of language barrier I cannot really assess
clearly what is the quality of pain but the quantity of pain
I can do...I have a problem with language, it is difficult
because of language barriers I cannot assess them properly"
Some nurses explain that it can be difficult to perform a
clear assessment because of unclear symptoms as well as the
presence of other diseases like diabetes mellitus. Also some
patients will have a silent attack and this silent attack
can delay the good assessment timing, therefore the management
also will be affected.
" Some patients will not
complain of pain, so this is a problem, they have a silent
attack like stroke. It is a silent symptom"
Nurses state the importance of having
good skills to do a proper assessment, otherwise lack of these
skills and experience will affect a patients' care negatively.
Also lacking experience is one of the obstacles that faces
nurses every day and make the situation most difficult.
"You know only thing
we lacking is experience, practice makes everything perfect"
Nurses face other difficulties when
they need to have consent for high-risk procedures or management
especially if a patient has no attendant or interpreter.
Although there is a pain scale for unconscious patients but
still some nurses are not aware about how to use the scale
and some of them will neglect the patient's pain. Another
obstacle occurs when a nurse neglects the patient's pain because
some though that patients malinger the pain.
"Because some patients who stay long time here, they
will malinger, they will say they still have pain even if
they do not have pain, sometime I intend to neglect their
pain"
Nurses express the need of more staff, either doctors or nurses
because they have shortage of staff that affects early assessment
and doing improper intervention.
In the chosen CCU the nurses handle about four patients at
a time and this under staffing makes it difficult for nurses
to do the required assessment. Moreover, the communication
with the doctors becomes difficult when they are busy with
many patients.
"Sometimes it is difficult
because here in CUU we should handle one to one ratio, but
we are under staffed"
Pressure at work and shortage of
staff can cause communication problems between nurses and
doctors. Other obstacles that interfere with pain assessment
is having uncooperative patients due to having severe pain.
On the other hand some patients deny having pain and this
will delay proper assessment and intervention.
"Sometime doctors
have many patients their mood will not be ok because of many
patients; some doctors will come and shout at us"
"Patients can deny the pain
even though a patient on severe pain will say mild"
Different approaches in pain assessment
Objective nursing assessments
of pain
Objective assessments include the procedures that nurses do
during nursing assessment, for example physical assessment
and evaluating diagnostic tests, and assessment of myocardial
infarction signs when a patient is admitted to the CCU. Nurses
will perform different diagnostic procedures and follow some
diagnostic tests to confirm the diagnosis of MI. The first
thing that nurses do is to check the severity of pain by using
different scales. One scale is the numerical scale that can
be used if a patient is conscious.
"If they are in severe pain you can see from the facial
expression, we assess the pain, how is the pain we have pain
score 1-10, we ask how much the pain"
Assessment of cardiac enzymes and
electrolytes are important tests that patients should have
in the CCU. Nurses will send the investigation to the lab
and follow up the result. When any abnormal result is occurred
the nurses refer to the physician for further orders. Furthermore,
nurses do the assessment of the electrocardiogram and almost
all nurses are able to read the ECG and interpret the diagnosis.
There are different signs and symptoms
that the nurses rely on to diagnose MI. Signs include chest
pain, vomiting, sweating and having abnormal reading of ECG.
Objective assessment of pain includes vital signs, doing ECG
and using different scales to assess the pain. If a patient
is conscious; nurses use the numerical scale (0-10) and if
the patient is unconscious nurses use the FLACC scale "Face,
Legs, Activity, Cry, Consolability".
" We assess the vital signs, ECG if there is ST elevation,
tachycardia, the patient is restless and he has abnormal behaviors.
We have FLACC assessment scale for unconscious patients every
two hours"
Doctors use invasive procedures for pain assessment like doing
catheterization to visualize entire arteries if there is any
block and this can help to diagnose MI by doctors in the CCU.
" We have coronary catheterization lab, and the doctor
is available so we will send the patient for catheterization
without medication" primary PTCA" and the patient
should have normal Creatinine test"
Subjective approaches of pain assessments
In this category nurses use subjective assessment of what
a patient verbalized during assessment and during taking the
patient's history. Assessment of pain by taking the patients'
history is very important. Nurses use Wong-Baker scale (0-10)
for conscious patients to assess verbalized pain by the patient.
" We have Wong-Baker FACES
pain rating scale and other one behavioral scale"
Nurses use alternative methods to
communicate with a patient and assess his needs if he cannot
talk for example using a piece of paper and help the patient
to write his needs. Moreover, nurses use a holistic assessment
approach to assess pain characteristics.
" We can ask the patient what
kind of pain, is it dull pain, where is the site of pain,
central chest pain, right side pain of chest, pain from chest
radiates to the right arm or at back, sometimes they will
not complain of chest pain they complain of abdominal pain"
Holistic approaches in pain management
Pharmacological therapies are used by doctors
The main treatment, which is used for patients with myocardial
infarction, is pharmacological therapy. Pharmacological therapies
include administration of thrombolytic therapy like Reteplase.
It depends on the type of MI and duration of pain, and nurses
can also give Oxygen by different modes.
"If a patient candidates
for thrombolytic therapy; before we use Reteplase but now
we use Alteplase, if pain between 6 hours we have special
protocol, and if pain more than 6 hours we have also a special
protocol...If they are in pain so we give Oxygen we can give
face mask or non re breathing mask if tolerated"
Doctors prescribe Pethidine as a common medication if patients
are in pain. Moreover, nurses use especial protocols to treat
acute myocardial infarction. This contains administration
of anti coagulants, O2, anti platelet and thrombolytic therapy.
" Usually in acute MI a doctor
will confirm first, we are following certain thrombolytic
protocol, we also started the anti coagulants Heparin and
Aspirin and Plavix loading dose, and Oxygen should be present"
Management of pain using MONA protocol,
includes "Morphine, Aspirin, O2 and Nitroglycerine, and
if a patient is still in pain they do Coronary Angiography.
Another treatment includes using intravenous fluids if needed
especially if a patient has low blood pressure. If pharmacological
medications did not relieve the patient's pain the doctor
will order an advance procedure like CAG.
"Like during hypotension also we can ask the doctor
to give IV fluid so quickly if ejection fraction (EF) is good
we can give bolus to increase blood pressure".
"Sometimes even if you give
Morphine and Pethidine but still the patient complains of
pain; the doctor will do Coronary Angiograph; and then a patient
will be ok, it is diagnostic and interventional procedure"
Non pharmacological interventions used by nurses
In a non-pharmacological approach; nurses use their skills
and provide independent nursing care like administer Oxygen
and put the patient in a comfortable position. Another independent
nursing care is to help the patient to do breathing exercises.
Some nurses find the use of diversional activities are helpful
and can reduce the patient's pain especially if the patient
is stable, like talking to patients and help the patient to
read something.
" Once a patient is stabilized
we can render independent nursing care like keep a patient
in a comfortable position, provide support, measures like
say to the patient he will be ok, we talk to the patient because
some patients will have anxiety and they are worry regarding
what will happen to them and he will be able to recover"
Other nurses are used to provide a patient with psychological
support and other spiritual care and the nurses feel this
support helps patients and relieves their stress. Furthermore,
nurses in the CCU enhance bed rest and provide necessary messaging
when a patient is in pain because some nurses believe messaging
could relieve the patient's pain.
" We nurses do psychological support, reassurance,
we encourage a patient to verbalize their pain and feeling,
we touch a patient, we being with a patient, talk to the patient,
it is very relieving"
Collaborative management in multi-
professional teams
Collaborative work between nurses and physicians is a
very important aspect that nurses mention especially in the
coronary care unit because they have serious cases that require
good team management all the time. Nurses are used to exchanging
their knowledge and information with their doctors, in order
to be updated with their information and to render good care.
" For me I know cardiologists
nowadays are available we can ask the doctor what type of
MI and if we can thrombolyse him if there is ST elevation"
Some nurses ask social workers for
help if they have any problem with patients in the CCU, especially
if a patient refuses to take the medication or refuses important
care. Another type of cooperation is to cooperate with the
patient's family and provide them with the necessary information
so they will be aware about the plan of their patient.
"Some patients are not cooperative, some patients
will not take the medication, and we cannot force them in
this situation we will ask the social workers to help"
" Doctors will explain to the family and we secure
the consent from the family and then administer thrombolytic
if a patient is ok"
Nurses provide good and cooperative management and it mainly
depends on the physicians' plans. Another form of cooperation
is the cooperation with the family of the patient and to help
them to participate in the patient's care.
" Sometime we cannot change
patients' position alone and do suction and we cannot ask
other staff because other staffs has patients also, we ask
also the attendant to help us"
Nurses explain that if the patient
needs advanced care in another center, a referral paper will
be sent and cooperative care will be provided.
" For CABG "Coronary Angio Bi-pass Graphy "we
send to another hospital"
DISCUSSION
Discussion of the method
In August 2012 the author did ten interviews; all of the interviews
were recorded and no problems occurred during the recording
of data. The interviewer used notes to document nurses' perceptions
regarding pain assessment and pain management. The author
did the interviews in different days and in different shifts,
for example the author met the nurses during the morning shift,
evening shift and during the night shift. Doing the interviews
in different shifts helps the author to meet nurses with different
experiences. The interviews took place in the coronary care
unit "CCU", and the place of the interviews had
been chosen by the participants.
In this study there was no drop out among the participants
since the author conducted the interviews immediately after
recruiting of the voluntary staff. After the selection of
participants; the author did the interviews separately with
each nurse alone with consideration to privacy. The author
did the analysis of data manually and the analysis was done
several times to get the proper themes that reflect the nurses'
perceptions. The study's transferability can be assured by
using the same criteria of the participants (Polit & Beck,
2008). However, this study is limited to ten nurses and it
does not represent all the nurses in coronary care units in
Saudi Arabia. It was conducted in one hospital because of
the time limit and this limits the generalizability of the
result. However, in qualitative studies there is no precise
rule for numbers of participants (Patton, 2002). The number
of participants in this study seemed to fulfill the aim of
the study.
Content analysis is a method which was used in this study.
Content analysis is a method to analyze the content of narrative
data (Polit and Beck, 1999). This method helped the author
to identify the main themes through breaking down the narrative
sentences to meaning units, then condensed meaning units and
had the main codes and themes according to Graneheim &
Lundman (2004). The author spent a long time reading and understanding
how to do content analysis and the process was checked several
times with the supervisor. To ensure the credibility of the
result a second person (the supervisor of this study) has
been involved to check the data analysis and discuss different
themes (Patton, 2002).
Discussion of the result
This study highlights the important aspects of pain assessment
and pain management for patients with myocardial infarction
in a coronary care unit (CCU). Three themes have been identified
which reflect nurses' perceptions in the chosen CCU when dealing
with myocardial infarction cases.
Dealing with patients who have myocardial infarction pain
is challenging
In this study the author observed that the result agrees with
other studies in the literature. Pain assessment and pain
management have different aspects with varied approaches.
The presence of obstacles and challenges are manifested as
important aspects in this study. In the literature by Morton
and Fontaine (2009); there are many challenges in a critical
care nursing, for instance dealing with critically ill patients,
different diagnoses, and cultural diversity among people,
multilingual staff and sophisticated technology. Some nurses
explained myocardial infarction diagnosis as a difficult situation
and there could be different components that could complicate
the situation and make the pain management difficult. Skrobik
(2008) states that pain assessment is challenging in critical
care units and it is one of the most common problems and stressors
in any critical care area including CCU.
According to Hadjistavropoulos and Craig (2004) and Morton
and Fontaine (2009) there are varied circumstances, which
interfere with pain assessment, for example acuity of the
patients' condition, altered level of consciousness, inability
of a patient to communicate pain and the patient's immobility.
This agrees with the nurses in this study who express different
factors that interfere with pain assessment that are making
the process most difficult. These factors include language
problems in that the patients and nurses had different languages,
which affect general care as nurses explain in this study.
In another study which has been done by Montes-Sandoval (1999)
and Shannon and Bucknall (2003) it is indicated that some
barriers affect pain assessment that include inability to
communicate with patients, presence of a complicated technology,
less nurses' knowledge and having limited time in doing patients
care. Having language barriers and communication difficulties
and less experienced staff are obstacles that interfere with
good management; this highlighted by the nurses in this study.
Results in the present study showed
that nurses perceived that lack of experience and language
problems interfere negatively with good pain assessment. In
the chosen CCU the majority of the staff is non-Arabic speaking
whereas patients are Arabic speaking and this is a big problem
for successful communication. Having problems with communication
can cause ineffective pain assessment and also can leadto
improper pain management. This agrees with Ge´linas
and Johnston (2007); they concluded in their study that some
factors interfere with pain assessment for instance the use
of sedation, mechanical ventilation and inability of patients
to communicate verbally. Another problem occurs when there
are complications of thrombolytic therapy as nurses mentioned
during pain management. In the literature; these complications
make the situations very difficult for staff to manage. In
addition to the presence of treatment complications there
are some cases with sudden deterioration. There are other
predisposing factors that restrain adequate pain assessment;
they include the presence of technology and the rapidly changing
situations of patients (Shannon & Bucknall, 2003; Puntillo,
Smith, Arai & Stotts, 2008).
Different approaches in pain assessment
Holistic assessment of pain characteristics includes the assessment
of pain, location, severity, duration, and relieving factors
as nurses experienced in this study. Chen and Zieve (2011)
mentioned that chest pain is the most common symptom of heart
attacks. However, some patients will present with other pain
like arm pain, shoulder, neck, teeth, jaw and back pain. In
this study some nurses explain that there are different signs
of myocardial infarction for example increasing of Troponin
I, abnormality of cardiac enzymes, and other symptoms, which
a patient presents with like sweating and vomiting. In a study
which has been done by Chen and Zieve (2011) they concluded
the same result that the characteristics of heart attack pain
will be as following; heavy chest, squeezing heavy pressure
on chest, anxiety, cough, dizziness, irregular heartbeats,
shortness of breath, sweating, nausea or vomiting.
Nurses in this study explain that patients in the CCU have
anxiety and stress during their admission in the hospital
and this needs proper assessment. Studies have been done by
(Montes-Sandoval, 1999; Shannon & Bucknall, 2003; McCarberg
et al., 2008) which indicate that unrelieved pain can negatively
impact a person's quality of life, causing activity life disturbances
like psychological distress; anxiety, depression and lack
of sleep. Nurses propose the use of some scales like Wong-Baker
scale for conscious patients to assess pain. Hadjistavropoulos
and Craig (2004) state the different approaches that have
been used in hospitals to assess pain clinically, for example
self-report, behavioral-observational methods and using different
scales. In this study nurses explain the use of different
scales including Ramsey scale for sedated patients, and other
pain scales depend on the patient's case. However, nurses
in the same department have different perceptions regarding
using the scale assessments as some of them were aware about
using different scales whereas some were not aware of those
scales. This indicates the need for education and improving
nurses' skills and information. Non-verbalizing patients were
not having the needed assessment because some nurses were
not aware about the FLACC scale, which is the scale used in
the chosen CCU for unconscious patients.
In this study some nurses use a piece of paper to assess the
patient's pain if a patient cannot talk so the nurses can
assess the patients' different needs and this is strongly
recommended. In literature patients who are not able to provide
a verbal self-report of pain with other signs (e.g., head
nodding, pointing to a scale), the use of a valid behavioral
pain scale is strongly recommended by Hadjistavropoulos &
Craig 2004; Ge´linas & Johnston, 2007; Puntillo,
Smith, Arai & Stotts, 2008; Gelinas, Arbour, Michaud,
Vaillant & Desjardin, 2011).
Holistic approaches in pain management
In this study management of pain includes using the MONA
protocol which includes Morphine, Oxygen, Aspirin and Nitroglycerine
besides using advanced technology if needed like doing interventional
Coronary Angiography. In literature if a patient with a heart
attack is stable with normal vital signs and the patient is
conscious, the patient can go for a coronary angiography test;
X-ray, which is used in this test helps to see how the blood
flows through the main arteries (Adam & Osborne, 2005;
National Institute for Health and Clinical Excellence, 2010).
Nurses mention that doctors only can prescribe Pethidine or
Morphine as narcotic drugs for pain. In a study, which has
been done by Shannon & Bucknall (2003) they state that
physicians are required to prescribe medications, including
analgesics and sedatives. Whereas a study that has been done
by (Hadjistavropoulos & Craig, 2004) shows that nurses'
driven protocol of pain management was effective in many cases.
Nurses in this study emphasize the importance of using non
pharmacological approaches like doing massaging; ask patients
to do deep breathing and using diversion activities to divert
a patient's attention from pain. Having non-pharmacological
interventions may help in alleviating patients' suffering
of pain and it increases quality of nursing care (Lindberg
& Engström, 2011).
Nurses verbalize their roles in pain
management that include non pharmacological interventions
as well as psychological support, reassurance, encouraging
patients to verbalize their pain and feeling, touching a patient,
being with a patient, talking to the patient, it is very relieving.
Hyden and Fields (2010) state that nurses are in a unique
position to implement the correct practice in CCU. Moreover,
bedside nurses have first-hand knowledge about compliance
to follow up patient care. However, some nurses in this study
may ignore patients' pain and they thought that patients are
malingering the pain, and so having good education about pain
assessment and management is a very important aspect in the
chosen CCU.
The author finds providing comfort
and support is very important during nursing care, especially
when patients are in pain and need management or support and
this agrees with many nurses in this study who verbalized
providing comfort for patients during pain. Using this theory
of comfort helps to release patients' suffering and distress;
it can also support the patients to experience a feeling of
comfort (Kolcaba, Tilton & Drouin, 2006).
Nurses in this study state the importance
of early recognition of myocardial infarction, which helps
early recovery. St Marie (2002) states that early recognition
of pain and proper intervention enhances good patient outcomes,
moreover; early recognition of pain-shortened hospital stay
and decreased costs. In this research there are different
approaches of pain management including pharmacological and
non-pharmacological treatment and this agrees with other studies.
Puntillo, Smith, Arai & Stotts (2008) concluded that the
management of pain includes pharmacologic treatment, non-pharmacologic
treatment, or a combination of both and nurses are expected
to develop the skill of balancing those treatment options.
Nurses in critical care areas should
be competent, knowledgeable and well trained to deal with
critically ill patients (Shannon & Bucknall, 2003). In
the current study; nurses explain the need of proper skills
and experience during assessment because patients' care depends
on nursing mainly. Adam and Osborne (2005) write that patients
who are admitted to coronary care areas need to have special
care, which is provided by well-trained personnel including
critical care nurses.
Critical care nurses and physicians
maintain themselves to have a strong commitment to pain relief
(Skrobik, 2008). In this study the result showed that nurses
perceived that they should manage pain quickly to save patients'
lives and especially if a patient develops any complication
for instance hypotension or bleeding. Furthermore, nurses
in this study cooperate with social workers and family of
patients in case they need further help and patient support.
Providing cooperative pain management by nurses and doctors
to improve patients' outcomes in the CCU is very important
as nurses believed. The presence of the doctor during pain
management is a very important aspect especially when giving
the thrombolytic therapy and this is to avoid complications
and poor outcomes that may occur during late treatment. Shannon
and Bucknall (2003) & Adam and Osborne (2005) state that
poor recognition of MI and lack of skills to recognize patients
with acute illness lead to poor outcomes for patients and
increases the mortality rate.
STUDY LIMITATIONS
This study includes ten critical
care nurses, moreover the study has been conducted in one
hospital, although with these limitations; the author got
saturated data that was rich to explain nurses' perceptions
when they care for patients with MI (Polit & Beck, 2008).
In qualitative studies it does not matter about the number
of participants as long as the researcher gets the saturated
data that answers the study aim (Patton, 2002).
NURSING IMPLICATIONS
This study has good implications in the nursing field. Pain
assessment and pain management are relevant areas in improving
nursing quality of care. Organizations' performance is measured
by the patients' satisfaction about nursing care. Therefore,
working to improve the aspect of patients' assessment and
management would participate in good patient outcomes. Nursing
education and further research is important in contemporary
nursing since the patients' care is the main concern in any
health organization.
CONCLUSION
In conclusion, this study aims to explore nurses' perceptions
regarding pain assessment and pain management for patients
with myocardial infarction in a coronary care unit in one
selected hospital. In the study, the CCU nurses practice pain
management by using the hospital protocols which may help
to relieve patients' suffering of pain. On the other hand,
some nurses lack the knowledge regarding the use of some pain
assessment scales and some nurses may neglect patient's pain
due to lacking the proper knowledge. Furthermore, non-verbalizing
patients, either unconscious patients or patients who cannot
talk, are more prone to receiving inadequate pain management.
Nurses' knowledge and information are very important because
nurses are in a critical position to assess and manage patients'
pain in coronary care units. Nurses in this study face difficulties
of communication with patients due to having language barriers
and the author recommends the department administration to
solve this current problem. Having language barriers delays
proper pain assessment and affects pain management. One solution
is to provide the department with interpreters and Arabic-speaking
staff who may participate in effective pain assessment and
pain management. Finally, providing nurses with good education
including some courses would enhance nurses' knowledge and
improve quality of nursing care. Further research is recommended
in this area, and including patients in further studies would
give a better result.
REFERENCES
Adam, S. A., & Osborne, S. (2005). Critical care nursing:
science and practice (2nd). New York: OXFORD university press
Blumgart, H. L., & Zoll,P. M. (1960). Pathologic Physiology
of Angina Pectoris and Acute Myocardial Infarction. Circulation
the Journal of American Heart Association, 22,301-307
Cambridge Dictionary Organization. (2012). Perception. Retrieved
May 9, 2012 from http://dictionary.cambridge.org/dictionary/business-english/perception
Chen, M. A., & Zieve, D. (2011). Heart attack: Myocardial
infarction; MI; Acute MI; ST-elevation myocardial infarction;
non-ST-elevation myocardial infarction. Retrieved May 5, 2012
from http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001246/
Edwards, H.E., Nash, R.E., Yates, P. M., Walsh, A. M., Fentiman,
B. J., McDowell, J.K., Skerman, H. M., Najman, J.M. (2001).
Improving pain management by nurses: a pilot peer intervention
program. Nursing and Health Sciences Journal, 3(1), 35-45
Elo, S., & Kynga, S H. (2008). The qualitative content
analysis process. Journal of Advanced Nursing, 62(1), 107-115
Funk, M. (2011). As Health Care Technology Advances: Benefits
and Risks. American Journal of Critical Care, 20 (4), 285-291.
Ge´linas, C., & Johnston, C. (2007). Pain Assessment
in the Critically Ill Ventilated Adult: Validation of the
Critical-Care Pain Observation Tool and Physiologic Indicators.
Clinical Journal of Pain, 23(6), 497-505
Gelinas, C., Arbour,C ., Michaud, C., Vaillant, F., &
Desjardin, S. (2011). Implementation of the critical-care
pain observation tool on pain assessment/management nursing
practices in an intensive care unit with nonverbal critically
ill adults: a before and after study. International Journal
of Nursing Studies, 48, 1495-1504.
Gelinas, C. (2007). Management of pain in cardiac surgery
ICU patients: Have we improved over time? Intensive and Critical
Care Nursing Journal, 23, 298-303
Glynn, G., & Ahern, M. (2000). Determinants of critical
care nurses' pain management behavior. Australian Critical
Care journal, 13(4), 144-151
Graneheim, U.H., &Lundman, B. (2004). Qualitative content
analysis in nursing research: concepts, procedures and measures
to achieve trustworthiness. Nurse Education Today, 24(2),
105-12.
Hadjistavropoulos, T., & Craig, K. D. (2004). Pain psychological
perspectives. Mahwah, New Jersey London: Lawrence Erlbaum
Associates, Inc (p.391)
Hsieh, H., & Shannon, S.H. (2005). Three Approaches to
Qualitative Content Analysis. Qualitative Health Research,
15 (9), 1277-1288
Hwang,S. Y., Ahn,Y.G. &Jeong, M.H.(2012). Atypical Symptom
Cluster Predicts a Higher Mortality in Patients With First-Time
Acute Myocardial Infarction. Korean Circulation Journal, 42,
16-22
Hyden, R., Fields, W. (2010). Improving the Acute Myocardial
Infarction Rapid Rule out Process. Journal of Nursing Care
Quality, 25(4), 313-319
International Council of Nurses. Code of ethics. Retrieved
June 4, 2012 from
http://www.icn.ch/images/stories/documents/about/icncode_english.pdf
Kolcaba, K., Tilton, C., & Drouin, C. (2006). Comfort
theory: A unifying framework to enhance the practice environment.
The Journal of Nursing Administration, 36(11), 538-543
Lindberg, J., & Engström, A. (2011). Critical Care
Nurses' Experiences: ''A Good Relationship with the Patient
is a Prerequisite for Successful Pain Relief Management. Pain
Management Nursing journal , 12(3), 163-172
Mann, E., & Carr, E. (2006). Pain management: essential
clinical skills for nurses. Australia: Blackwell Publishing
Marieb, E. N. (2006). Essentials of human anatomy and physiology
(8th ed). San Francisco: Pearson Benjamin Cummings
McCarberg, B, H., Nicholson, B. D., Todd, K. H., Palmer, T.,
& Penles, L. (2008). The Impact of Pain on Quality of
Life and the Unmet Needs of Pain Management: Results from
Pain Sufferers and Physicians Participating in an Internet
Survey. American Journal of Therapeutics,15, 312-320
Medical libraries: Mercer the University school of Medicine.
(2012). Myocardial infarction. Retrieved October 2, 2012 from
http://library.med.utah.edu/WebPath/TUTORIAL/MYOCARD/MYOCARD.html
Montes-Sandoval, L. (1999). An analysis of the concept of
pain. Journal of Advanced Nursing, 29(4), 935- 941
Morton, P. G. & Fontaine, D. K. (2009). Critical Care
Nursing: a holistic approach (9th). China: Lippincott Williams
& Wilkins.
National Institute for Health and Clinical Excellence {NICE}.
(2010). Unstable angina and NSTEMI: The early management of
unstable angina and non-ST-segment-elevation myocardial infarction.
Retrieved May 14, 2012 from http://publications.nice.org.uk/unstable-angina-and-nstemi-cg94/guidance#management-strategies
National Open University of Nigeria [NOUN]. (2009). Perception
and conflict. Retrieved May 9, 2012 fromhttp://www.nou.edu.ng/noun/NOUN_OCL/pdf/pdf2/PERCEPTION%20&%20CONFLICT%20PCR%20276.pdf
O'Connor, l. (1995). Pain assessment by patients and nurses,
and nurses' notes on it, in early acute myocardial infarction.
Part 2. Intensive and Critical Care Nursing Journal, II, 283-292
Patton, Q.M. (2002). Qualitative Evaluation and Research Methods.
(3rd ed). London: SAGE Publications, Inc
Polit, D. F., & Beck, C. T. (2008). Nursing research:
Generating and assessing evidence for nursing practice (8th
Ed.). Philadelphia: Lippincott Williams & Wilkins.
Puntillo, K. A., Smith, D., Arai, S., & Stotts, N. (2008).
Critical care nurses provide their perspectives of patients'
symptoms in intensive care units. Heart and lung; the journal
of acute and critical care, 37(6), 466-475
Shannon, K., & Bucknall, T. (2003). Pain assessment in
critical care: what have we learnt from research? Intensive
and Critical Care Nursing, 19, 154-
162
Skrobik, Y. (2008). Pain may be inevitable; inadequate management
is not. Critical Care journal, 12:142 (Doi: 10.1186/cc6865).
St Marie, B. (2002). Core Curriculum for Pain Management Nursing:
American Society of Pain Management Nurses. USA: W.B. Saunders
Trotter, R., Gallagher, R. & Donoghue, J.(2011). Care
of Patients with Coronary Heart Disease Anxiety in patients
undergoing percutaneous coronary interventions. The journal
of heart and lung, 40, 185-192
Valen, V. R., Vuuren, H. V., Domburg, R. T. V., Woerd, D.
V. D., Hofland, J., Bogers, A. (2012). Pain management after
cardiac surgery: experience with a nurse-driven pain protocol.
European Journal of Cardiovascular Nursing, 11(1), 62 -69
Van de Werf, F., Bax, J., Betriu, A., Blomstrom-Lundqvist,
C., & Filippo Crea, F.et al. (2008). Management of acute
myocardial infarction in patients presenting with persistent
ST-segment elevation. European Heart Journal, 29, 2909-2945
World Medical Association [WMA]. (2012). Declaration of Helsinki-Ethical
Principle for Medical Research Involving Human Subjects. Retrieved
June 4, 2012 from http://www.wma.net/en/30publications/10policies/b3
|
 |




