| |
October
2013 - Volume 7, Issue 5
The effects
of earplug on perception of sleep in patients of coronary
care unit (CCU)

|
 ( (
|
Fateme Mashayekhi
(1)
Mansour Arab (2)
Farokh Abazari (2)
Foozieh Rafati (1)
Hossein Rafiei (3,4)
(1) Department of
Medical- Surgical Nursing, School of Nursing and Midwifery,
Jiroft University of Medical Sciences, Jiroft, Iran
(2) Department of Medical- Surgical Nursing, School
of Nursing and Midwifery,
Kerman University of Medical Sciences, Kerman, Iran
(3) Social Health Determinants Research Center,
Shahrekord University of Medical Sciences, Shahrekord,
Iran
(4) Department of Intensive and Critical Care, School
of Nursing and Midwifery,
Shahrekord University of Medical Sciences, Shahrekord,
Iran
Correspondence:
Hossein Rafiei
Department of Intensive and Critical Care, School of
Nursing and Midwifery, Shahrekord University of Medical
Sciences, Shahrekord, Iran
Email: Hosseinrafiei21@yahoo.com
|
 |
|
Abstract
Background and Aim: Sleep deprivation can affect
the health of patients and may tend to effect recovery
from illness. This study aims to assess the effects
of earplug on perception of sleep in patients who are
admitted to CCU.
Methods: A single group crossover design was
used. Thirty patients were recruited from a CCU in Iran
during March to July 2012. Using Verran and Snyder-Halpern
Sleep Scale (VSH Sleep Scale), perception of patients
sleep with and without usage of ear plug were evaluated.
This tool consists of 16 items that include three main
sleep sub scales: disturbance, effectiveness, and supplementation.
Finding: Of the 30 patients, 17 were men. The
mean age of patients was 51±18.1 years. Mean
time of patients' nocturnal sleep was 6.6± 1.1
hours. Using ear plug statistically significantly increased
the quality of sleep in three subscales (disturbance,
effectiveness, and supplementation) (P<0.05).
Conclusion: Patients in coronary care unit (CCU)
are at risk of sleep deprivation. The use of ear plug
is an easy and cheap method to improve the perception
and quality of sleep in CCU patients.
Key words: Ear plug, sleep perception, CCU, patient
|
INTRODUCTION
Although the function of sleep is not clear, it is generally
accepted that lack of sleep can affect the health of patients
and may tend to delay recovery from illness (Dogan et al.,
2005; Higgins et al., 2007; Jafarian Amiri et al., 2012; Venkateshiah
et al., 2012). In general, hospitalization can affect patients'
quality of sleep (Reid, 2001; Venkateshiah et al., 2012).
It can be related to environmental, physiological and psychological
factors (Dogan et al., 2005; Honkus, 2003; Pellatt, 2007).
Sleep disturbances in critically ill patients are defined
as of insufficient duration or stages of sleep that result
in discomfort and interference with quality of life (Tastan
et al., 2010; Urden et al., 2010). One group of hospitalized
patients that encounter sleep problems and symptoms of sleep
disturbances are patients with cardiovascular disease (Tastan
et al., 2010). Environmental stimuli in the critical care
unit could be disruptive for patients' sleep (Honkus, 2003;
Richardson et al; 2007; Tastan et al., 2010). The environmental
stimulus that is most often cited in the literature as disturbing
sleep, is noise (Freedman et al., 1999; Meyer et al; 1994;
Redding et al., 1977). Sustained noise impairs quality and
quantity of sleep and increases adrenocorticotrophic hormone
release, triggering the stress response which reduces motivation
and cognition. (Intensive care nursing)
Although most sleep disorders in CCU patients could be treated
by using pharmacological methods; (Daneshmandi et al., 2012;
Moeini et al., 2010; Neyse et al., 2011) however, non-pharmacological
methods still remain important and a less expensive way for
increasing quality of sleep in hospitalized CCU patients (Moeini
et al., 2010; Neyse et al., 2011). Van Rompaey et al., in
2012, studied the effects of reduction of sound during the
night with use of earplugs in the prevention of intensive
care unit delirium (Van Rompaey et al., 2012). They reported
that use of earplugs may be a useful instrument in the prevention
of confusion or delirium, especially within 48 hours after
admission (Van Rompaey et al., 2012). Scotto et al., evaluated
the use of earplug on the subjective experience of sleep for
critically ill patients. They reported that use of earplug
improved the subjective experience of sleep in this group
of patients (Scotto et al., 2009). In the study of Hu et al.,
the effects of earplugs and eye masks on nocturnal sleep,
level of urine melatonin and cortisol in healthy subjects
exposed to simulated intensive care unit environment were
evaluated (Hu et al., 2010). They reported that the use of
earplugs and eye masks may increase rapid eye movement (REM)
time, decrease REM latency, cause less arousal and elevate
levels of melatonin in urine (Hu et al., 2010).
The importance of sleep is not a new concept. However, sleep
disruption continues to be a problem in hospitals and with
the emphasis on the use of non-pharmacologic methods for improving
patients' sleep quality in CCU, few studies have been performed
in this area. The aim of this study was to examine the effects
of earplug on perception of sleep in CCU patients.
MATERIAL AND METHODS
The study was conducted during the period of March to July
2012 in Kerman in Iran. Ethical approval was obtained from
the research ethical centre of the Kerman University of Medical
Science and head of Kerman hospital. A single group crossover
design was used. The sample was composed of 30 patients who
were admitted in CCU. This unit has 8 beds in 8 separated
rooms. According to hospital protocol, at 22:30 every night,
all lights were turned off for helping patients to have a
better sleep. A "night's sleep" is considered as
the period from when the person tried to sleep until waking
up in the morning (Bergamasco et al., 2007). Written consent
was obtained from each participant. Before obtaining the patients'
consent, the research was comprehensively described to each
patient, and they were assured that their information will
be used only for research purposes. Inclusion criteria of
the study were: aged more than 18 years, being alert enough
to respond to the questionnaire, having a stable hemodynamic
situation, no history of hearing disorders, and who had not
previously used an ear plug at sleep time. Patients with previous
sleep disorders (acute or chronic), patients with history
of mental disorder and patients who used narcotics, sedative,
psychiatric and analgesic drugs, were excluded. The participants
were randomly divided into two groups: with ear plug (group
1) or without ear plug (group 2) in sleeping time in the first
night after admission to CCU. In the second night, patients
in the two groups were changed and group 2 used ear plugs
and patients in group 1 did not use ear plugs. Patients' room
and beds were similar in both nights for every patient. Correct
use of ear plug by patients was controlled by researchers
working in CCU.
Data collection tools in this study were Verran and Snyder-Halpern
Sleep Scale (VSH Sleep Scale). Using this questionnaire, patients
provided an assessment of the quality of their previous night's
sleep. This tool consists of 16 items which include three
main sleep sub scales: "disturbance' (interruptions and
delays in sleep), "effectiveness' (how well sleep refreshed
the individual), and "supplementation' (napping). Disturbance
comprises items measuring subscales of fragmentation (interruption
of sleep) and "latency' (delay in getting to sleep).
Effectiveness comprises the subscales of "quality' (restfulness
and depth of sleep), and "length' (hours of sleep while
in bed). Supplementation contains four items about naps and
falling back asleep after morning awakenings. Each characteristic
is measured using a 100 mm visual analogue scale and the total
score for the primary outcome of sleep disturbance is a sum
of the scores from each scale (total score maximum 700). A
lower total score on this scale indicates a lower degree of
sleep disturbance. For effectiveness, higher scores indicate
better sleep (Bergamasco et al., 2007; Call-Schmidt et al.,
2003; Frighetto et al., 2004; Snyder-Halpern et al., 1987).
In order to translate the English version of VAS into Farsi,
the standard forward-backward procedure was applied. Translation
of the items and the response categories was independently
performed by six professional translators and then temporary
versions were provided. Later, they were back translated into
English and after a careful cultural adaptation, the final
versions were provided. The validity of questionnaire has
been assessed through a content validity discussion. Scholars
of statistics, physicians and nurses have reviewed the content
of the questionnaire. To reassess the reliability of the translated
questionnaire alpha coefficients of internal consistency were
used. The alpha coefficient for questionnaire was 0·91.
Data were analyzed with use of descriptive statistics (mean
and standard deviation (SD)), Chi squared test and paired
t-test. All statistical analyses were performed using SPSS
software (v15.0; PASW Statistics). A P value of less than
0.05 was considered as statistically significant.
RESULTS
Of the 30 patients, 17 were men. The mean age of patients
was 51±18.1 years. Table 1 shows patient's demographic
characteristics. Mean time of patients' nocturnal sleep was
6.8 ± 1.15 hour. Mean score of sub scale "disturbance"
before and after intervention was 140.90± 55.6 and
89.83± 52.1 respectively. In this sub scale, most change
before and after use of ear plug was related to item "wake
after sleep onset". In sub scale "effectiveness",
mean score of sleep quality was 255.33± 41.1 before
intervention and 291.50± 38.9 after intervention. In
this sub scale, most change before and after use of ear plug
was related to item "sleep sufficiency evaluation".
Results of paired t-test showed significant difference in
mean score of sub scales "effectiveness" and "disturbance"
before and after use of ear plug (p<0.05). Mean score of
sub scale "supplementation" before and after intervention
was 25.50± 27 and 40.80± 23.4 respectively.
In this sub scale, most change before and after use of ear
plug was related to item "wake after final arousal".
Results of paired t-test showed significant difference in
sub scale of "supplementation" before and after
use of ear plug (p<0.05). Mean scores of three sub scales
have been shown in detail in Table 2 and Figure 1.
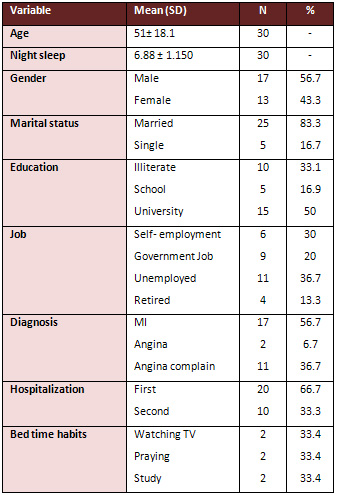
Table 1: Patients' demographic characteristics
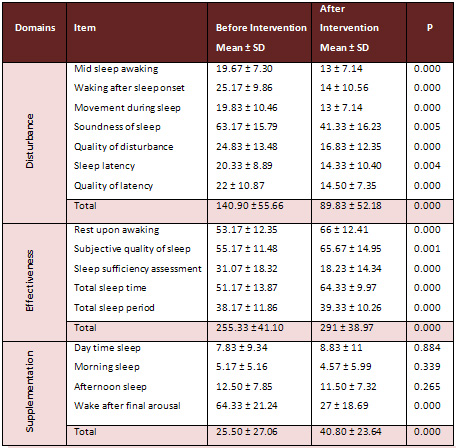
Table 2: Sleep Quality Score before and after intervention
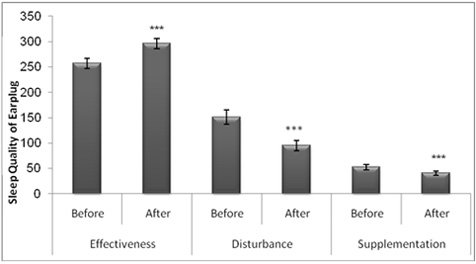
Figure 1: Mean of sleep perception score before and after
the intervention
CONCLUSION
In order to evaluate the effects of ear plug on perception
of sleep in CCU patients, this study has been conducted. Our
results showed that in general, patient's perception of sleep
significantly improved after use of ear plug in this group
of patients. Quality of sleep in hospitalized patients should
be a routine part of patients' assessment such as vital signs,
because the patients sleep quality may reveal more information
about the patients' overall well-being (Young et al., 2008).
One important group of patients who may have higher risk of
sleep disturbance is patients with heart diseases (Norra et
al., 2012). Zeighami et al., in 2013 reported that patients
who suffer from heart disease, may have many problems in sleeping
(Zeighami et al., 2013). The two most common sleep problems
reported by Zeighami et al., were insomnia and sleep apnea
(Zeighami et al., 2013). They also reported that factors such
as weight loss, smoking cessation, control and treatment of
chronic diseases and control of drug side effects could decrease
sleep problems in this group of patients (Zeighami et al.,
2013).
High level of sound may considerably affect the quality of
patients' sleep (Tastan et al., 2010). Zolfaghari et al.,
in 2013 investigated the effects of environmental modification
on quality of sleep among CCU patients (Zolfaghari et al.,
2013). They reported that interventions of decreasing excessive
environmental light and noise; such as turning off extra lights,
use of bulbs with low light, decreasing the alarm sounds levels
throughout the night, decreasing level of telephone ringtone
during night and educating staff regarding the control of
environmental excessive light and noise have improved the
patient's nocturnal sleep in CCU (Zolfaghari et al., 2013).
In 2010, Neyse et al., surveyed the effects of earplug and
eye mask on quality of patients' sleep in critical care unit
(Neyse et al., 2010). Similar to our finding, Neyse et al.,
reported that the use of earplug and eye mask could improve
patients' sleep in critical care unit. (Neyse et al., 2010).
Hu et al., in 2010 studied the effects of earplug and eye
mask on sleep of healthy subjects exposed to simulated intensive
care unit (ICU) noise and light (Hu et al., 2010). They reported
that use of earplugs and eye masks may increase REM sleep
and decrease REM latency and cause fewer arousals (Hu et al.,
2010). In agreement with our finding, Richardson et al., reported
that use of non-pharmacological methods could improve patients'
sleep quality in CCU (Richardson et al., 2003). They reported
that the use of relaxation and imagery is effective in improving
the sleep of the critically ill adult patients. (Richardson
et al., 2003) They also stated that men have a better response
to this intervention. (Richardson et al., 2003)
Healing cannot occur without a good night's sleep (Dunn et
al., 2010; Tastan et al., 2010). Sleep deficit and sleep without
a refreshing and restorative function may increase the risk
of recurrent events in patients with heart diseases (Leineweber
et al., 2003). Members of the health care team, especially
nurses, should pay more attention to satisfying the need of
rest and sleep for critically ill patients (Neyse et al.,
2010; Li et al., 2011). Nurses should assess patient sleep
patterns routinely during hospitalization and then evaluate
the need for sleep promotion strategies (Ünsal et al.,
2012). Results of the present study confirmed that quality
of nocturnal sleep in CCU patients was significantly improved
after use of ear plug. Therefore, using ear plugs at night
time is a cheap and comfortable method, which has been recommended
for improving the quality of
sleep in CCU patients.
REFERENCES
1 - Bergamasco EC, Cruz DALM. (2007). Adaptation of the visual
analog sleep scales to Portuguese. Rev Latino-am Enfermagem;
15: 998-1004.
2 - Call-Schmidt TA, Richardson SJ. (2003). Prevalence of
sleep disturbance and its relationship to pain in adults with
chronic pain. Pain Manag Nurs; 4: 3.
3 - Daneshmandi M, Neiseh F, SadeghiShermeh M, Ebadi A. (2012).
Effect of eye mask on sleep quality in patients with acute
coronary syndrome. Journal of Caring Sciences; 1: 135-143.
4 - Dogan O, Ertekin S, Dogan S. (2005). Sleep quality in
hospitalized patients. J Clin Nurs; 14: 107-113.
5 - Dunn H, Anderson AM, Hill PD. (2010). Nighttime lighting
in intensive care units. Crit Care Nurse; 30: 31-37.
6 - Eliassen KN, Hopstock LA. (2011). Sleep promotion in the
intensive care unit - A survey of nurses' interventions. Intensive
Crit Care Nurs; 27: 138-142.
7 - Freedman NS, Kotzer N, Schwab RJ. (1999). Patient perception
of sleep quality and etiology of sleep disruption in the intensive
care unit. Am J Respir Crit Care Med;159:1155-1162.
8 - Frighetto L, Marra C, Bandali SH, Wilbur K, Naumann T,
Jewesson P. (2004). An assessment of quality of sleep and
the use of drugs with sedating properties in hospitalized
adult patients. Health Qual Life Outcomes; 2: 17.
9 - Higgins PA, Winkelman C, Lipson AR, Guo SE, Rodgers J.
(2007). Light measurement in the hospital: a comparison of
two methods. Res Nurs Health; 30: 120-128.
10 - Honkus VL. (2003). Sleep deprivation in critical care
units. Crit Care Nurs Quart ; 26: 179-189.
11 - Hu RF, Jiang XY, Zeng YM, Chen XY, Zhang YH. (2010).
Effects of earplugs and eye masks on nocturnal sleep, melatonin
and cortisol in a simulated intensive care unit environment.
Crit Care; 14 :R66.
12 - Jafarian Amiri SR, Zabihi A, Babaie Asl F, Sefidchian
A, Bijanee A. (2012). Sleep quality and associated factors
in hospitalized patients in Babol, Iran. Hormozgan Medical
Journal; 15: 144-151.
13 - Lane T, East LA. Sleep disruption experienced by surgical
patients in an acute hospital. (2008). Br J Nurs; 17: 766-771.
14 - Leineweber C, Kecklund G, Janszky I, Akerstedt T, Orth-Gomér
K. (2003). Poor sleep increases the prospective risk for recurrent
events in middle-aged women with coronary disease. The Stockholm
Female Coronary Risk Study. J Psychosom Res; 54: 121-127.
15 - Li SY, Wang T, Wu SFV, Liang SY, Tung HH. (2011). Efficacy
of controlling night-time noise and activities to improve
patients' sleep quality in a surgical intensive care unit.
J Clin Nursing; 20: 396-407.
16 - Meyer, T., S. Eveloff, M. Bauer, W. Schwartz, N. Hill,
and R. Millman. (1994). Adverse environmental conditions in
the respiratory and medical ICU settings. Chest; 105:1211-1216.
17 - Moeini M, Khadibi M, Bekhradi R, Mahmoudian SA, Nazari
F. (2010). Effect of aromatherapy on the quality of sleep
in ischemic heart disease patients hospitalized in intensive
care units of heart hospitals of the Isfahan University of
Medical Sciences. Iran J Nurs Midwifery Res; 15: 234-239.
18 - Neyse F, Daneshmandi M, Sadeghi Sharme M, Ebadi A. (2011).
The effect of earplugs on sleep quality in patients with acute
coronary syndrome. Iran J Crit Care; 4: 127- 134.
19 - Norra C, Kummer J, Boecker M, Skobel E, Schauerte P,
Wirtz M, Gauggel S, Forkmann T. (2012). Poor sleep quality
is associated with depressive symptoms in patients with heart
disease. Int J Behav Med; 19 : 526-534.
20 - Redding, J., T. Hargest, and S. Minsky. (1977). How noisy
is intensive care? Crit Care Med; 5:275-276.
21 - Reid E. (2001). Factors affecting how patients sleep
in the hospital environment. Br J Nurs; 10: 912-915.
22 - Richardson A, Allsop M, Coghill E, Turnock C. (2007).
Earplugs and eye masks: do they improve critical care patients'
sleep? Nurs Crit Care; 12: 278-286.
23 - Richardson S. (2003). Effects of relaxation and imagery
on the sleep of critically ill adults. Dimens Crit Care Nurs;
22: 182-190.
24 - Scotto C J, McClusky C, Spillan S, Kimmel J. (2009).
Earplugs improve patients' subjective experience of sleep
in critical care. Nurs Crit Care; 14: 180-184.
25 - Snyder-Halpern R, Verran JA. (1987). Instrumentation
to describe subjective sleep characteristics in healthy subjects.
Res Nurs Health; 10: 155-163.
26 - Tastan S, Unver V, Iyigun E, Itisoy A. (2010). Study
on the effects of intensive care environment on sleep state
of patients. Anatol J Clin Investig; 4: 5-10.
27 - Ünsal A, Demir G. (2012). Evaluation of sleep quality
and fatigue in hospitalized patients. International Journal
of Caring Sciences; 5: 311-319.
28 - Urden L D, Stacy K M, Lough M E. (2010). Critical Care
Nursing Diagnosis and Management 5th ed. St Louis, Mosby;
567-687.
29 - Van Rompaey B, Elseviers MM, Drom WV, Fromont V, Jorens
PG. (2012). The effect of earplugs during the night on the
onset of delirium and sleep perception: a randomized controlled
trial in intensive care patients. Crit Care; 16: R73.
30 - Venkateshiah SB, Collop NA. (2012). Sleep and sleep disorders
in the hospital. Chest; 141:1337-1345.
31 - Woodrow P. Intensive Care Nursing a Framework for Practice.
2nd ed . London,
Rutledge; 2006: 23-25.
32 - Young J S, Bourgeois J A, Hilty D M, Hardin K A. (2008).
Sleep in hospitalized medical patients, Part 1: Factors affecting
sleep. J Hosp Med; 3: 473-482.
33 - Zeighami MSh, Shahparian M. (2013). Evaluation of sleep
problems and its associated factors in male patients with
systolic heart failure. Ghom Journal of Medical Science; 6:
64-73.
34 - Zolfaghari M, Farokhnezhad Afshar P, Asadi Noghabi AA,
Ajri Khameslou M. (2013). Modification of environmental factors
on quality of sleep among patients admitted to CCU. Hayat;
18: 61-68.
|
 |




