| |
April
2013 - Volume 7, Issue 2
Chemotherapy
Spill Management Policy: Policy Analysis

|

(
|
Bilal S. H. Badr
Naga (1)
Majd. T. Mrayyan (2)
(1)
Bilal S. H. Badr Naga, RN, MSNs
The Hashemite University
(2) Majd. T. Mrayyan, RN, MSc, PhD, Professor
The Hashemite University
Correspondence:
Bilal S. H. Badr Naga,
RN MSNs,
The Hashemite University
Amman, Jordan
Email:
Bilal_badrnaga@yahoo.com
|
 |
|
Abstract
There are many different chemotherapeutic agents
used in the treatment course of cancer patients. Chemotherapeutic
agents have been classified as hazardous by the National
Institute for Occupational Safety and Health. Chemotherapeutics
agents are therapeutic agents which are known to be
toxic to cells through their action on cell reproduction
and are primarily intended for the treatment of neoplastic
disorders. Chemotherapy agents have two unique features;
the first is the low therapeutic indexes, which places
patients at an increased risk for medication errors;
the second, is they are considered hazardous drugs,
which place patients and health care providers at risk
for environmental exposure. Accidental spill of chemotherapy
agents may occur during manufacture, transport, distribution,
receipt, storage, preparation, and administration, as
well as during waste handling and equipment maintenance
and repair. As nurses and health care providers are
involved in preparation and administration of chemotherapeutic
agents, they may expose themselves to hazardous effects
that have been reported in several studies.
Key words: policy, chemotherapy, spill, cancer,
hazardous drugs.
|
Introduction
There are many different chemotherapeutic agents used in the
treatment course of cancer patients (WHO, 2012). Chemotherapeutic
agents have been classified as hazardous by the National Institute
for Occupational Safety and Health (NIOSH, 2004). Chemotherapeutic
agents are therapeutic agents which are known to be toxic
to cells through their action on cell reproduction and are
primarily intended for the treatment of neoplastic disorders
(Amiruddin, 2002). Chemotherapy agents have two unique features;
the first is the low therapeutic indexes, which places patients
at an increased risk for medication errors, the second is
they are considered hazardous drugs, which place patients
and health care providers at risk for environmental exposure
(Griffin, 2003).
Accidental spill of chemotherapy agents may occur during manufacture,
transport, distribution, receipt, storage, preparation, and
administration, as well as during waste handling and equipment
maintenance and repair (Amiruddin, 2002). As nurses and health
care providers are involved in preparation and administration
of chemotherapeutic agents they may expose themselves to hazardous
effects that have been reported in several studies.
Kyprianou, Kapsou, Raftopoulos, and Soteriades, (2010) reported
that nurses and health care providers complain of acute symptoms
related to exposure of chemotherapeutic agents such as skin
irritation, sore throat, cough, dizziness, headache, hair
loss, allergic reaction, diarrhea, nausea, and vomiting. Also,
frequent abortion has been reported by health care providers
who were exposed to chemotherapeutic agents (Martin, 2003;
Kyprianou, et al. 2010); and disabilities in the offspring
of nurses who handled chemotherapy during pregnancy.
Furthermore, Martin, (2003) and Smith, (2012) (?showed) in
their studies an increased rate of certain cancers in health
care providers (HCP), as a result of handling chemotherapeutic
agents specifically, when mixing and administering these agents,
accidental spills, sprays, chemo bag punctures and frequent
contact with hazardous drugs.
Centers for Disease Control CDC (2010), confirm that chemotherapeutic
agents continue to contaminate the work spaces where they
are used, and in some cases it is still being found in the
urine of those who handle them, despite knowledge of safety
precautions. Also, the National Institute for Occupational
Safety and Health (NIOSH, 2004) reports that exposure to chemotherapeutic
agents have not been determined by a reliable method (NIOSH,
2004). Furthermore, in the United Kingdom, the Greater Manchester
and Cheshire Cancer Network GMCCN, (2009 ) reported that the
health care workers who are involved in the handling of chemotherapy
drugs, and if not adequately protected, will absorb harmful
quantities of these drugs through their skin. Health care
institutions who use these agents developed chemotherapy spill
policy to guide nurses and other health care providers in
order to protect them from the dangerous health consequences
that may result from spillage. Thus, it is significant to
nurses, stakeholders, and administrators to review and analyze
the chemotherapy spill policy.
Purpose
The purpose of this paper is to review and analyze the chemotherapy
spill policy in one tertiary care hospital (Islamic hospital)
in order to identify issues and propose alternative solutions.
Suggested alternatives will be discussed with regard to strength,
weaknesses, administrative ease, cost, benefit, effectiveness,
equity, legality and the acceptability of the policy.
Islamic Hospital Background
Islamic hospital (IH) was established in 1982 in Amman as
a private hospital. The total capacity of the hospital is
250 beds. Islamic hospital is considered the first teaching
hospital in the Jordanian private health sector. Although,
there are many oncology patients treated in IH, and chemotherapy
management approach is considered one of the main procedures
done to cancer patients, there is no special department for
oncology patients, but there is a policy for chemotherapy
spill management.
Islamic Hospital Chemotherapy Spill Management Policy Description
The purpose of chemotherapy spill management in IH is to manage
chemotherapy spill. This policy is applicable for all hospital
staff. The purpose, scope, definitions, policy statement,
responsibility, and procedure are clearly stated in the policy
manual. Also, the policy steps are stated as following: (1)
Chemotherapy spill kits to be kept in all departments where
chemotherapy is administered; (2) Clean up is a nursing responsibility
and second clean up will be performed by housekeeping; (3)
If linen is involved in the spill place it in a double blue
bag; and (4) If chemotherapy agent comes in contact with the
skin, the area must be washed with a good amount of water
and soap for at least 5 minutes. The implementation of the
policy is the responsibility of the head of the department
and the continuous education department.
Verify, define and detail the problem
Issue Statement
Does the chemotherapy spill policy in Islamic hospital provide
a safe environment and prevent hazardous effects to health
care workers?
Scope of Problem
Exposure to chemotherapeutic agents may occur during preparation,
administration, and disposal which may impose an occupational
hazard for health care provider and workers (CNSA, 2003).
The chemotherapy spillage not only affects the healthcare
providers, but also, patients receiving chemotherapy and their
family members, can also be exposed to the hazards of chemotherapy
drugs when they handle contaminated equipment or body fluids
(CNSA, 2003).
Research studies have identified chemotherapeutic agents in
the urine of the workers and has negative genetic responses
in the health care providers (Valanis, et al. 1993; Thomas,
2006). Hazards of exposure to chemotherapeutic agents can
occur by various activities such as direct contact, when preparing,
administering, cleaning, inhalation, storage and disposal
of chemotherapy waste. Thomas, Melissa, & McDiarmid, (2006
) and Polovich, (2004). In a study done by Mason (2003) to
detect the level of the chemotherapy drug after collecting
a sample from the outside of chemotherapy bags prepared in
the pharmacy and delivered to nursing station for administration,
Mason reported that when touching the bag of chemotherapy
without proper chemotherapy protection equipment, exposed
the nurses to chemotherapy. Mason also reported that no contamination
was detected on the bag of chemotherapy when received from
the pharmacy; the contamination happened in the pharmacy during
preparation and the contamination was not seen by the nurses
(Mas on, 2003). This shows the spillage may happen in any
stage of preparation or administration.
Moreover, chemotherapeutic agents may be used for diseases
other than cancer, such as Lupus, and multiple sclerosis (Polovich,
2004). In some hospitals these drugs are being administered
by nurses without proper training or being chemotherapy certified
which may increase exposure to chemotherapeutic agents for
healthcare providers (Polovich, 2004).
Health Impact
There are many adverse health problems caused by exposure
to chemotherapeutic agents especially to health care providers
who handle them or work in the surrounding setting of chemotherapy
administration (NIOSH, 2007). Acute side effects of exposure
to chemotherapeutic agents included skin irritation, sore
throat, cough, headache, hair loss, allergic reaction, diarrhea,
nausea, and vomiting (Kyprianou, Kapsou, Raftopoulos, and
Soteriades, 2010; NIOSH, 2007).
Also, infertility, miscarriage, preterm labor, and frequent
abortion have been reported by female health care providers
who exposed to chemotherapeutic agents (Martin, 2005; Kyprianou,
Kapsou, Raftopoulos, & Soteriades. 2010). In addition,
disabilities were found in the offspring of nurses who handled
chemotherapy during their employment (Martin, 2005). Furthermore,
Fransman (2007) reported that health care providers who handled
chemotherapeutic agents and are exposed to these agents took
a longer time to have children than other health care providers
who were not exposed to chemotherapeutic agents.
Many research studies confirmed that chemotherapeutic agents
have been found in the urine of health care providers who
handled chemotherapeutic agents, thus, there is an increased
risk of cancer among health care workers (Wick, 2003; Connor,
2006; NIOSH, 2007). These findings raised the question of
adherence to spillage policy or effectiveness of policy for
safe handling of chemotherapeutic agents.
Economic Impact
Chemotherapy has been administered in hospitals or clinics
used to treat cancer patients via intravenous infusion and
recently there has been an increase in the use of self-administration
of oral chemotherapy at home. Although, using oral chemotherapy
at home helps in decreasing the cost and use of health resources,
it may increase the risk of exposure to chemotherapy spillage
during administration if patients do not strictly adhere to
safety precautions (Aisner, 2007; Weingart, Brown, Bach, &
et al. 2008). Thus, compliance with strict policy and procedure
is very important to prevent the potential health risk due
to exposure, which may have a negative economic impact on
patients and their families to manage the adverse effects
of chemotherapy exposure.
There is a lot of expenditure on illness and injuries to health
employees, families, and the surrounding environment. The
impact may be financially and emotionally, which involves
follow-up testing, treatment and anxiety and stress. The ultimate
goal in any health care institution is to protect the staff
from the risks of chemotherapy spillage that can leave them
out of action for months, or even permanently. The International
Labour Organization (ILO, 2003) estimated that the cost of
global work - related injuries and illness accounts for 4%
of the world's gross domestic product. Employers face costly
early retirement, loss of skilled staff, and absenteeism,
due to work-related accidents and diseases (Giuffrida, Lunes,
& Savedoff, 2002). Also, Christopher Landrigan et al.
(2004) reported that occupational hazard that results from
unsafe workplaces affects the healthcare institution by increasing
the cost and reducing ability to provide services. Moreover,
Erinn and colleagues (2012) reported that reducing chemotherapy
spillage by health care providers and workers can save more
than 600,000 dollars every year in Canada. Thus effective
implementation of chemotherapy drug spill policy will help
decrease the cost, time and effort lost. Ultimately, decision
makers must consider such costs as investment, not losing
money. Health care institutions would have to value the significant
expense to comply with this policy and the real cost must
be weighed against the potential high cost of the treatment
of the health care worker.
Legal and Ethical Impact
From the ethical point view, health care workers do not wish
to see unnecessary injuries or illness occurring (ILO, 2003).
Ethical challenges in occupational health include issues related
to privacy of employees's health information, balancing of
cost and benefits, health screening, surveillance of employees,
and employees adaptation to health protection programs and
policy related issues (Rogers, 2012).
National Institute of Occupational Safety and Health (NIOSH,
2007) demonstrated that healthcare institutions have poor
laws and regulations that examine and analyze the cause of
chemotherapy spill issues and its sources, to prevent recurrence.
Also, NIOSH assured that every health care institution must
have a comprehensive safety program for controlling workplace
exposure to chemotherapeutic agents that must include training,
work practices, and personal protective equipment (NIOSH,
2004). Failure to maintain and provide the necessary equipment
is a legal issue. Moreover, NIOSH, (2004) reported that reproductive
risks have been associated with exposure to hazardous drugs
and an alternative duty should be offered to individuals who
are pregnant, or breast-feeding. All workers who handle hazardous
drugs should be routinely monitored in a medical surveillance
program (NIOSH, 2004).
Limited resources may stand as a barrier in the road of implementation
of chemotherapy spill policy; this is a legal and ethical
issue that may face health care professionals, thus it is
a duty to all health care institutions to present all necessary
resources to protect staff and patients from the side effects
of chemotherapeutic agents. It is also the duty of the health
care institution to develop strict measures to assess and
evaluate staff adherence to the policy and procedures who
handled these chemotherapeutic agents, in particular, chemotherapy
spill policy, otherwise it implies a legal and ethical behavior.
Who is concerned? Stakeholders
To discuss the issue of chemotherapeutic agents spillage,
all stakeholders who have a direct or indirect relationship
and are affected by the chemotherapy spillage issue, should
be involved. The governments, healthcare institutions, healthcare
professional/workers and medical industry should have a common
interest, goal, and work together to achieve the intended
goals.
Engaging with stakeholders, to develop well considered policy
that reflects diverse perspectives in order to enhance the
health and well-being of the people and prevent all unwanted
negative effects of chemotherapy spillage, it has been necessary
to develop a policy for preventive measures to be taken during
the preparation and administration of chemotherapeutic agents
and managing of chemotherapy spill during occurrence. In Jordan,
each health care institution develops a policy to promote
safety and ensure the quality of care. The decision makers
(stakeholders) who should be involved in formulating the chemotherapy
spill policy is a shared team that encompasses the government
(Ministry of Health), health care providers and workers, medical
industries, and the health care institution.
At the health institutional level, there is a need to adopt
policies that respond to the needs of patients, health practitioners
and other staff. It is the responsibility of the health care
institution to maintain the physical environment; service
coordination and continuity of care; multi-disciplinary collaboration
and partnerships, patient and staff education and training;
monitoring and measuring safe, quality and ethical services.
During monitoring the application of policy by health care
workers, is to encourage staff to report the incidents, not
for disciplinary action but for identifying problems and finding
solutions.
At the level of health care workers, building a stronger evidence
base on ways to improve health care and the health system
itself to achieve better health outcomes, satisfaction of
policy and ensure adherence to standards of care; and public
accountability for maintenance of professional standards achieves
a culture of quality and system improvement and not destructive
litigation and blame. Monitoring and addressing health care
workers' concerns about health care quality is imperative.
Also every health care worker is responsible in terms of policy
application and should be acquainted with an advanced training
and educational program that relates to chemotherapy usage
to prevent occurrence of spillage and the ability to handle
the spillage of chemotherapy in a safe manner according to
the policy.
At the level of the government, a supportive health system
will ensure that interventions implemented at the health institution,
health practitioner and health consumer levels are effective
and the performance evaluation systems have relevant policies.
In addition there is a need to build a stronger evidence base
on ways to improve health care and the health system itself
to achieve better health outcomes, and ensure the strengthening
of the monitoring of professional standards.
At the level of the medical industry, there are well-defined
regulations for manufacturers and distributors to ensure safe
transport and handling of chemotherapy drugs., although the
initial step for safe handling of chemotherapy agents begins
with the manufacturer. Follow up with new materials, resources
and information regarding chemotherapeutic agents should be
updated and provided to all stakeholders. The stakeholder's
needs, services provided and desired outcomes are clarified
in Table (1).
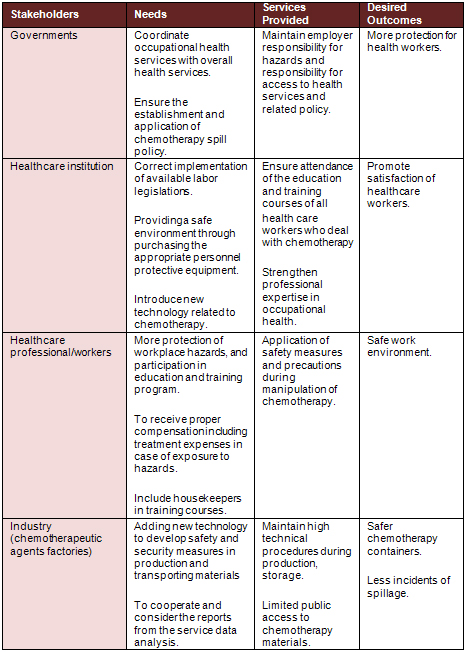
Table 1: Stakeholder of Chemotherapy Spill Management Policy
Policy Analysis
Before analyzing the current chemotherapy spill policy for
Islamic hospital, I gathered information and resource materials
such as policies from national and international health organizations.
To identify the gaps in this existing policy, I consulted
with the concerned staff in Islamic hospital to ensure that
appropriate personnel protective equipment (PPE) was identified
for use in the hospital and to identify issues in chemotherapy
policy, in addition to searching for policy issues through
books, publications, and research data, to develop solutions
to the policy issue; the advantages and disadvantages of potential
policy solutions; provide advice based on detailed analysis
of the spillage issues; and generate recommendations to address
the issue.
Policy Evaluation
In order to evaluate the chemotherapy spill policy we should
identify the major missing factors that lead to occupational
hazards at work place, then find the best alternatives that
may strengthen the policy and protect the health care providers
from hazards of chemotherapy spill exposure.
There are many problems during the evaluation process such
as: lack of statistical data base, absence of national health
information system regarding incident reporting, lack of information
regarding the effectiveness of implementation of such policy
on the health workers, and lack of sharing information among
different health sectors. Thus, the governmental and private
health sectors must work together in order to establish a
national health statistical system, and national incident
reporting system. This will help occupational health researchers;
disseminate findings and recommendations, and establish unified
training material. Also, this collaboration may help in minimizing
the number of injured health workers which is the main goal
of spill management policy. Occupational health and safety
legislation must be frequently reviewed and updated accordingly.
Alternatives
The most important issues are the lack of training and educational
programs for the health workers; poor or absence of safe working
practices; personal protective equipment (PPE); technology
use; medical surveillance and research support. Training and
educational programs are one of the most important alternatives
that should be implemented. All mentioned proposed alternatives
will be evaluated in terms of administrative ease, cost and
benefits, effectiveness, equity, and legality. Table (2) summarizes
the alternative solutions that may help in controlling and
minimizing health hazards associated with chemotherapy spillage.
A. Training and Education
Effective training and education regarding related precautions
is an important aspect in dealing withworkplace hazards. Such
training should be incorporated in all relevant educational
programs for healthcare employees. Personnel who are relatively
new to the healthcare environment are amongst those most at
risk. Performing continuous follow-up and development of occupational
health and safety is a very important step. Conducting of
regular refresher training courses may help experienced healthcare
workers, who have developed a negative attitude and consider
such risks as normal and expected, to change their behavior.
Such educational programs should clearly focus on risks of
exposure based on strong evidence from research findings.
Staff with minimal experience or no experience may be responsible
for handling hazardous drugs in units or areas that do not
normally care for cancer patients with chemotherapy management.
Specific training is required to prepare those staff before
assigning them to such a procedure (Brown et al., 2001). In
the case of staff shortage, administrators and supervisors
must provide appropriate and qualified staff who are able
to accomplish the new assignment safely. When chemotherapy
administration is an exclusive service, such as in oncology
infusion areas, providing fully cross-trained staff can be
problematic (Polovich, 2004).
When new information becomes available, it should be provided
immediately to employees. When a different job assignment
involves new risks, the employee should receive fresh training
and information about the hazards. Performing prevention programs
to prevent hazards is a primary prevention strategy (Polovich,
2004). Also, each healthcare facility should have an effective
reporting system in order to be able to assess the level of
illness and injuries related and to measure the benefits of
preventative measures taken.
B. Safe Working Practices
Each health care facility should establish policies and associated
procedures to reduce the incidence and severity of the health
risks that the health care professional may encounter if there
is no clear policy to be followed. Training and education
of staff needs to be reinforced with working policies and
procedures that are implemented in day -to-day routines. Also,
a healthy working environment and safety activities should
be maintained. Cooperation and collaboration should be maintained
among employers and health care providers. Health care professionals
have the right to participate in decisions concerning their
own work, particularly, concerns about occupational health
and safety.
C. Technology Use
Improved education, training and attention to working practices
cannot alone eliminate injuries. However, medical device technology
exists today to protect medical staff from unintentional injuries.
Medical devices are available with additional safety features
to prevent injuries.
D. Medical Surveillance
All workers who handle hazardous drugs should be routinely
monitored in a medical surveillance program (ASHP, 2006).
Medical surveillance involves the collection and interpretation
of data for the purpose of detecting changes in the health
status of working populations (ASHP, 2006). Medical surveillance
programs involve assessment and documentation of symptom complaints,
physical findings, and laboratory values (such as a blood
count) to determine whether there is a deviation from the
expected norms. Limited resources may preclude the implementation
of a comprehensive medical surveillance program for health
care workers who are exposed to hazardous drugs. In the absence
of an institutional medical surveillance program, workers
are encouraged to inform their personal health care providers
of their occupation and possible hazardous drug exposure when
obtaining routine medical care (ASHP, 2006).
E. Research Support
Governments are responsible and have the authority to develop
policies, guidelines, and to control work hazards by offering
resources in order to prevent occupational health hazards.
Also, the government is responsible for establishing a national
health information center to provide knowledge and information
related to occupational health hazards to deal with chemotherapeutic
drugs in different stages of handling.
Click
here for Table 2: Alternative solutions
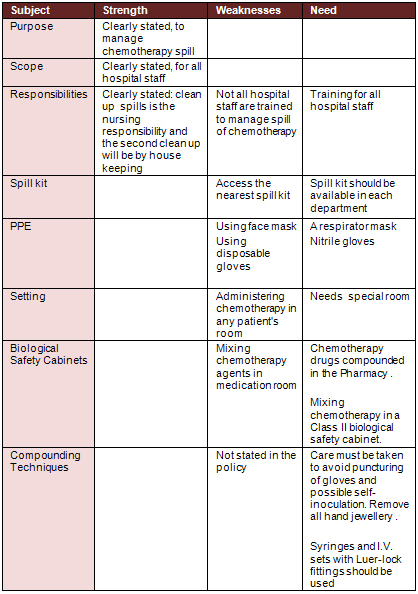
Table 3: Strength and weaknesses of Islamic hospital chemotherapy
spill policy
Discussion
Many chemotherapeutic drugs and other hazardous agents used
in the treatment of cancer patients pose a clear health danger
to healthcare workers who deal in preparation and administration
of these agents as well as the disposal of resulting waste
products (Polovich, 2004; Gambrell, 2006). Adopting safe-handling
practices, including the use of personal protective equipment,
engineering controls, and other new systems for safely preparing
and administering these agents, can help minimize the risk
of exposure to workers involved in drug therapy (NIOSH, 2004).
Martens, and Suh-Priest (2007) reported that oncology nurses
who are responsible for containment of spills during chemotherapy
administration have knowledge deficits and the need for practice
changes. It was found that the current chemotherapy policy
was outdated and needed to be revised. There are too many
proposed solutions that significantly reduce the risk of exposure
to chemotherapy which include developing training and educational
programs; establishing appropriate policies and working procedures;
using available protection technologies and building solid
base knowledge from related research. Ongoing training in
the safety of handling hazardous materials is required for
all involved personnel, which may reflect a job satisfaction
that may prevent the causes of spillage problems.
The cost to the health services when implementing effective
chemotherapy drug spill policy will decrease. Decision makers
must consider such costs as value adding not losing money.
Healthcare institutions would have to consider the expense
to comply with this policy because the cost of the consequences
of chemotherapy spillage on employee is more (ILO, 2003; Giuffrida,
Lunes, & Savedoff, 2002). There is a clear legal and ethical
obligation on employers to anticipate and manage risk, and
to provide safe working conditions and equipment for healthcare
workers.
This paper only proposes brief of alternative ideas to reduce
hazards of chemotherapy spill in the work place. Beyond the
ethical considerations, there is a growing body of law that
requires employers to combat risks at source. This paper may
help and influence the development of further intervention
strategies or further research to find alternative strategies
for reducing such hazards of chemotherapy spill. Every healthcare
institution must establish chemotherapy spill management policy
and related procedures to protect the institution and their
employers from health, economic and legal issues that may
arise. Periodic evaluation of the chemotherapy spill policy
may help in identifying the gaps that may lead to potential
risks and help in preventing these hazards.
Implementation, Monitoring and Evaluation
The purpose of this policy analysis is to review and analyze
the chemotherapy spill policy of the Islamic hospital and
provide them with information, and findings of the related
policy analysis, which help for potential change. In the policy
implementation phase, it is important to evaluate alternatives,
and choose the best alternatives to attain the desired goals.
The recommendations are intended to be applied to all departments
in Islamic hospital who are involved in handling chemotherapeutic
agents and may be exposed to hazards through chemotherapy
spillage. Islamic hospital stakeholders should have access
to the proposed recommendations. I will disseminate the report
to relevant stakeholders. Few changes need to be added or
modified to guide practice and policy change.
Monitoring the effectiveness and consequences of the policy
is required to consider how it is operating and whether it
is achieving the desired results. Evaluation of policy seeks
to relate and assess the connections between actual policies
and changes in the areas they are supposed to be influencing.
Islamic hospital and other health care institutions are highly
concerned about developing and reviewing chemotherapy policies
and procedures that may affect the health of employers.
Based on policy analysis process, the suggested plan will
include the following actions: (1)
• Increase awareness and perception of the stakeholders
about the chemotherapy spill policy and procedure based on
research through workshops, and disseminating of recommendations,
(2)
• Recommend to designate a multidisciplinary committee
of health professionals for assuring compliance with the chemotherapy
spill policy and procedures (3)
• Raise the issue of legislation regarding chemotherapy
to all concerned governmental and nongovernmental organization.
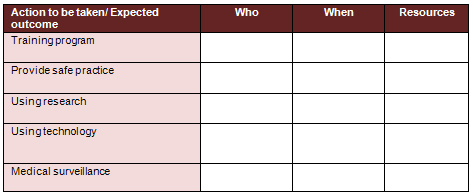 Table
4: Develop an action plan to implement the selected alternative.
An action plan identifies tasks, timelines, resources, and
responsibilities Table
4: Develop an action plan to implement the selected alternative.
An action plan identifies tasks, timelines, resources, and
responsibilities
Recommendations
A number of stakeholders are involved in handling chemotherapeutic
agents at various stages. Recommendations for safe handling
by these stakeholders are outlined in the following sections.
1. Manufacturers and Distributors
There are well-defined regulations for manufacturers and distributors
to ensure safe transport and handling of chemotherapy drugs,
although the initial step for safe handling of chemotherapy
agents begins with the manufacturer.
Appropriate packaging could minimize the handling of chemotherapy
drugs by health care providers and patients, thus contributing
to safer handling. This includes clear labeling on the outside
of the package indicating that the agent is cytotoxic. Additional
recommendations for manufacturers and distributors are listed
in Table 5. Health care professionals are encouraged to reinforce
the importance of these points to stakeholders and regulatory
agencies whenever possible.
2. Health Care Providers
Health care providers have a major responsibility in ensuring
safe handling of chemotherapeutic agents. Because of the significance
of this responsibility, health care providers should be appropriately
trained, ensure that their knowledge is current with developments
in the field, and follow all applicable discipline-specific
guidelines when handling chemotherapeutic agents. See other
recommendations in Table 6.
2. A. Training
Health care professionals should attend orientation programs
and routine training courses specific to their roles. They
should also complete competencies associated with these training
programs, along with an accompanying assessment for licensing
qualification if applicable. The training programs should
be approved by an oncology organization or appropriate local
organizations.
In addition, within a health care institution, a primary educator
should be established as a source of referral and continued
education for training health care professionals on chemotherapy.
This would ensure that patients receive consistent education,
training, and monitoring across the multidisciplinary team.
Health care workers should be trained and competent to treat
individuals accidently exposed to chemotherapeutic agents
and on the disposal of cytotoxic medications. All clinical
staff who are likely to come in contact with oral chemotherapeutic
agents or with waste from patients who have received these
agents (e.g. clerks, hygiene workers, and sanitation workers)
should undergo appropriate training. The latter point of training
non-health care professional staff was important because this
recommendation is not included in the Islamic hospital policy.
A list of training recommendations for health care providers
is shown in Table 6.
2. B. Storage and Handling
When handling chemotherapeutic agents, health care providers
must adhere to good practice as defined by procedures manual
and policy. Key recommendations are outlined in Table 6.
Minimize or eliminate any role of pregnant staff in handling
chemotherapy agents. Clean non-disposable materials exposed
to chemotherapy drugs. This includes trays, tools, and surfaces.
Cleaning of the tools and surfaces exposed to these agents
has been limited to washing the items and area thoroughly
with soap and water, 70% alcohol, or sodium hypochlorite;
in some settings, no cleaning occurs. The risk for contamination
of other medications and patient exposure could be significant.
2. C. Patient Counseling
Health care professionals should provide patients and caregivers
with education and training to ensure their understanding
of safe handling procedures as well as thorough knowledge
of proper administration of all medications. Patient literature
and other educational materials should be monitored and evaluated
to ensure that current and accurate information is being delivered.
Clear dosing instructions should be provided, including what
to do when a dose is skipped or when vomiting of a dose (spillage)
occurs.
During refill of prescriptions, any potential medication and
food interactions must be reassessed and discussed with the
patient or caregiver. The patient should be made aware of
the required monitoring arrangements by being provided with
access to the written protocol and treatment plan from the
institution where the treatment was initiated. Patients who
are pregnant or breast-feeding should be counseled on recommended
medications and their risk-benefit profiles.
3. Patients and Caregivers
Recommendations for patients and caregivers are included in
Table 7. Caregivers should understand all information given
to patients, including the transport, storage, dispensing,
and disposal requirements to ensure safe handling.
They must work with the patient and health care provider to
ensure appropriate dosing for patients in their care and report
any treatment-related adverse effects. Caregivers who are
pregnant or breast-feeding, or children, should not handle
any chemotherapy agents or waste products. Finally, to further
ensure the safety of these individuals and others in the patient's
home, guidelines from Australia and Canada recommend that
patient's clothes and bed linen be handled with gloves and
washed separately from other items and that toilets be double-flushed
after use, during and four to seven days after discontinuing
chemotherapy. Because drugs may be eliminated from the body
as active or inactive metabolites in sweat, saliva, urine,
or stool for five to seven half-lives, these recommendations
were important and should be implemented.
These recommendations are adopted from the American Society
of Health Systems Pharmacists: ASHP guidelines on handling
hazardous drugs, 2010.
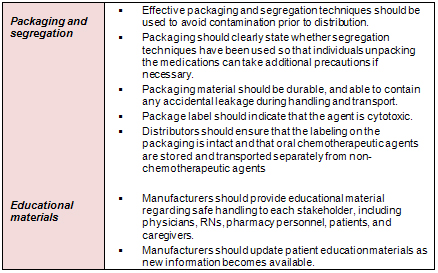
Table 5: Recommendations for Manufacturers and Distributors
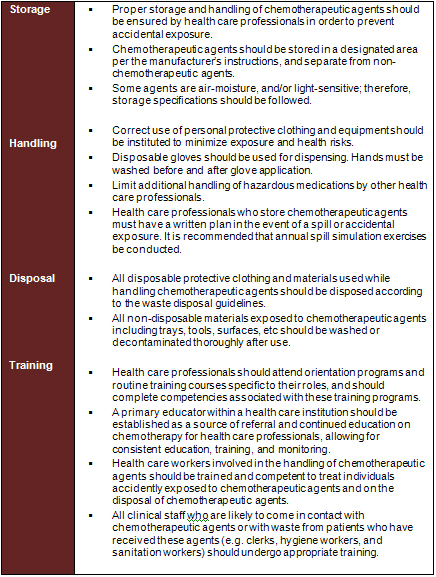
Table 6: Recommendations for Health Care Provider
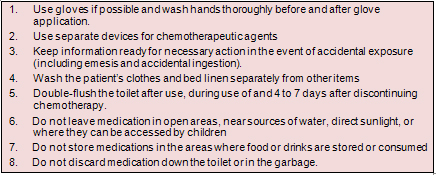
Table 7: Specific Recommendations for Patients and Caregivers
Conclusion
A lot of health care professionals and workers are exposed
to hazardous agents on a daily base, and many of them seriously
injured. Several measures and efforts can be done to reduce
such risks factors that lead to such hazards. In this paper,
I identified gaps in existing policy for the safe handling
of spilled chemotherapeutic agents. This paper only proposes
some alternative ideas to enhance and eliminate the factors
that influence the reduction of chemotherapy spill. First,
the proposed recommendations are relevant to multiple stakeholders,
beginning with the manufacturer. In addition, this recommendation
has been developed based on international policy and best
practices, and compiled to fill the gaps in existing policy.
Therefore, these recommendations may help health care institutions
to change or reshape their chemotherapy spill policy to maintain
safe handling of chemotherapy to health workers and practices.
All stakeholders should follow established guidelines when
handling chemotherapeutic agents and continually review and
assess their standards and compliance with agreed procedures.
This paper may influence the development of further intervention
strategies or further research to find alternative strategies
for reducing spillages of chemotherapeutic agents that are
aimed to prevent, or at least reduce, the occupational hazards
in the future. In addition, all facilities that handle chemotherapy
agents should evaluate the policy and practice annually or
as necessary. The major implementation strategies are to enhance
training efforts, modify standardization and support related
research, and sharing recommendations at national level and
improving the quality of the medical industry related to handling
chemotherapeutic agents, as well as in the work place, is
important.
References
Aisner, J. (2007). Overview of the changing paradigm in cancer
treatment: Oral chemotherapy. American Journal Health System
Pharm. 64 (5), 4-7
American Society of Health-System Pharmacists. (2010). ASHP
guidelines on handling hazardous drugs. American Journal of
Health-System Pharmacy, 63, 1172-1193
American Society of Hospital Pharmacists (ASHP, 1990). Technical
assistance bulletin on handling cytotoxic and hazardous drugs.
American Journal of Hospital Pharmacists, 47:1033-1049.
Amiruddin, A. (2002). Managing cytotoxic drugs. Malaysian
Journal of Pharm.1(3),63-68
Brown, K.A., Esper, P., Kelleher, L.O., O'Neill, J.E.B., Polovich,
M., & White, J.M. (2001). Chemotherapy and biotherapy
guidelines and recommendations for practice. Pittsburgh, PA:
Oncology Nursing Society.
CNSA. (2003). Position statement on the minimum education
and safety requirements for RNs involved in the administration
of cytotoxic drugs, p.1. Retrieved November 2012, from http://www.cnsa.org.au/publications_policies_pub.htm
Connor, T., McDiarmid, M. (2006). Preventing occupational
exposures to antineoplastic drugs in health care settings.
CA Cancer J Clin,56, 354-356.
Erinn, C., Rowe, M.S., Scott, W., Savage, M.S., William, A.,
Rutala, M. (2012). Economic and microbiologic evaluation of
single-dose vial extension for hazardous drugs. American Society
of Clinical Oncology, vol. 12
Fransman, W., Roeleeld, N., Peelen, S., deKort, W., Kromhout,
H., Heederik, D (2007). Nurses with dermal exposure to antineoplastic
drugs: Reproductive Outcomes. Epidemiology, 18 (1), 112-119.
Giuffrida, A., Lunes, R.F. & Savedoff, W.D. (2002). Occupational
risks in Latin America & the Caribbean: Economic &
Health Dimension. Health Policy & Planning 17 (3): 235-246
Griffin, E. (2003). Safety considerations and safe handling
of oral chemotherapy agents. Clin J Oncol Nurs.7, (6), 25-29
GMCCN, (2009). Policy & Procedure for the management of
cytotoxic chemotherapy Spillage policy. Retrieved on 20/11/2012
from www.gmccn.nhs.uk/Spillage Policy.
International Labour Organization, (2003). ILO standards-related
activities in the area of
occupational safety and health: Report VI retrieved on 20/11/2012
from http://www.ilo.org/public/english/standards/relm/ilc/ilc91/pdf/rep-vi.pdf
Kyprianou, M., Kapsou, M., Raftopoulos, V., & Soteriades,
E.S. (2010). Knowledge, attitudes and beliefs of Cypriot nurses
on the handling of antineoplastic agents. European Journal
of Oncology Nursing, 14, 278-282
Landrigan, C.P., Rothschild, J.M., Cronin, J.W., Kaushal,
R., Burdick, E., Katz, J.T. et al. (2004). Effect of reducing
interns' Work hours on serious medical errors in intensive
care units. The New England Journal of Medicine, 28
Martens, J. & Suh-Priest, C. (2007). The safe handling
of chemotherapy. Oncology Nursing Forum, 34, (2), 532
Martin, S. (2003). Chemotherapy handling and effects among
nurses and their offspring. Columbia University, New York,
NY.
Martin, S. (2005). Chemotherapy handling and effects among
nurses and their offspring . Oncology Nursing Forum, 32, 425.
Mason, H., Morton, J., Garfitt, S., Iqbal, S., Jones, K. (2003).
Cytotoxic Drug Contamination on the Outside of Vials Delivered
to a Hospital Pharmacy. Annal of Occup Hygiene, 47 (8), 681-685.
National Institute for Occupational Safety and Health (NIOS,
2004). Preventing occupational exposure to anti-neoplastic
and other hazardous drugs in health care settings. Retrieved
November 2012 from www.cdc.gov/niosh/docs/2004-165/
National Institute of Occupational Safety and Health (NIOSH,
2007). Occupational exposure to antineoplastic agent, Retrieved
November 19, 2012, from (http://www.ecd.gov/niosh/topics/antineoplastic/default.html)
Polovich, M. (2004). Safe handling of hazardous drugs. Online
Journal of Issues in Nursing. 9, (3), 5.
Rogers, B. (2012). Occupational and Environmental Health Nursing:
Ethics and Professionalism. Work-place Health & Safety
Journal, 60 ,( 4), 177-181
Smith, C. (2012). Oncology nurses get cancer from handing
chemo drugs. Retrieved on 15/12/2012 from http://seattletimes.com/html/localnews/2012327665_chemo11.html
Thomas, H. (2006). Preventing occupational exposures to antineoplastic
drugs in health care settings. CA Cancer journal for clinicians,
56, 354-365
Valanis, B. G., Vollmer, W. M., Labuhn, K. T., Glass, A. G.
(1993). Association of antineoplastic drug handling with acute
adverse effects in pharmacy personnel. American Journal Hosp
Pharm, 50, 455-462.
Weingart, S., Brown, E., Bach, P., & et al (2008). NCCN
Task Force Report: Oral
chemotherapy. Journal of National Cancer Network. 6, (3),
1-14.
Wick, C., Slawson, M.H., Jorgenson, J.A., Tyler, L.S. (2003).
Using a closed-system protective device to reduce personnel
exposure to antineoplastic agents. Am J
Health Syst Pharm, 60, 2314-2320.
World Health Organization (WHO, 2012). Cancer control: knowledge
into action. Retrieved
on 20/11/2012 from http://www.who.int/cancer/modules/en/index.html
|
 |




