| |
August
2013 - Volume 7, Issue 4
Educating Nurses
for Person-Centered Care

|
 ( (
|
Lois Thornton
Correspondence:
Lois Thornton
University of Calgary, Qatar
P. O. Box 23133, Doha, Qatar
Telephone: 974 4406 5319
Fax: 974 4482 5608
Email: lethornt@ucalgary.edu.qa
|
 |
|
Abstract
Background and Objectives: A person-centered
model for long-term institutional care of elder persons
is supportive of Arab societal values and Islamic beliefs.
Four workshops were conducted for nurse leaders from
long term care facilities in Qatar with the overall
objective of initiating a practice culture change which
would result in evidence of more person-centered care
practices.
Methods: Workshops were
held weekly for 4 weeks. Participants were 23 nurse
managers and supervisors from 3 long term residential
facilities in Doha, Qatar. Evaluation forms were completed
by participants after each workshop and a focus group
was conducted with the participants from one facility
12 weeks after the workshops.
Results: Participants
reported increased person-centered care practices on
their units. These practices began with staff coming
together around shared values and philosophy and included:
more attention to residents' personal preferences; inclusion
of residents and family in decision-making and social
activities; individualized care plans; therapeutic relationships.
Discussion: More research
into the implementation of care models that support
Arab religious and family values is essential to meet
the growing need for high quality long term residential
care in the Arab Gulf region.
Key Words: Person-centered
care, education, elders, Arab society
|
Introduction:
Long term institutionalized care for elderly persons is a
relatively new phenomenon in the Arab Gulf countries. However,
the Arab population, like the rest of the world, is aging
and the need for residential long term care for older people
is likely to increase. This need will be exacerbated by societal
and family changes related to modernization that will challenge
traditional expectations of the family to provide all care
for its aging members (1,2). At present, residential long
term care in the region tends to be clinically and task oriented
(3, 4). In most instances, care is provided by expatriate
nurses of diverse backgrounds and various levels of knowledge
of Arab culture and society. Models of care that support Arab
religious and family values are required for high quality
long term care alternatives for Arab families.
A person-centered model of care ensures the dignity of the
individual and encourages involvement of the family unit in
care, in keeping with Arab societal values and Islamic belief.
As well, a person-centered care framework could bring a diverse
nursing workforce together around a common philosophy and
consistent approach, leading to improved health outcomes and
satisfaction of residents and their families (5). Person-centeredness
is grounded in shared values and expressed through the workplace
culture of care.
This paper describes an educational program provided to nurse
leaders of long term care facilities in Qatar. Utilizing the
person-centered care framework developed by McCormack &
McCance (5), the intent of the program was to introduce nursing
leaders to the concepts of person-centered care, investigate
shared values that facilitate the development of a person-centered
workplace culture, and analyze how the shared values are operationalized
in practice. By directing the education to nursing leaders,
it was hoped that they would transfer their knowledge to front-line
staff, encourage action learning by staff and begin a culture
shift on their units.
Literature
Review
Nursing has long identified person-centeredness, holism and
individualized care as being integral to quality patient care.
However, within the past decade the international focus on
humanizing health and social services has precipitated extensive
research and literature on the meaning of the term "person-centered"
and its implications for nursing and other healthcare practice
(5). Person centered care has been defined as "an approach
to practice that is established through the formation and
fostering of therapeutic relationships between all care providers,
patients, and others significant to them" (6, p. 3) and
is based on the values of respect for persons, self determination,
mutual respect and understanding.
McCormack & McCance (5) purport that nurses often experience
person-centered "moments" in their practice, but
that sustained cultures of care where person-centeredness
is commonly recognized as the "way of doing business"
are infrequently encountered. Person-centered cultures of
practice are cultivated through a commitment to change and
careful attention to the care environment and care processes
as well as the attributes and skills of the nurses providing
care (5).
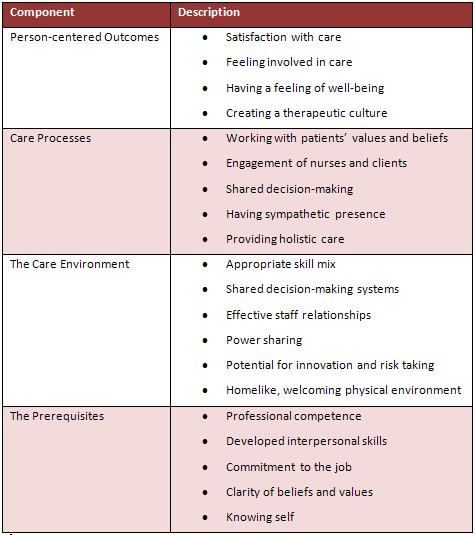
The framework developed by McCormack & McCance (5) places
person-centered outcomes at the center of a care environment
that is supportive of person-centered care processes and dependent
on the person-centered skills and attributes of the care givers.
The outcomes-satisfaction with care, involvement in care,
feeling of well-being, creation of a therapeutic culture-are
achieved only when there is synergy between the care processes,
the care environment and the attributes of the carers. Person-centered
processes describe the approaches taken in completing the
tasks of care: working with patients' beliefs and values;
shared decision making; engagement of nurse and client; having
sympathetic presence, and providing holistic care (5). The
processes can happen only in an environment that supports
shared decision-making, power sharing, and effective staff
relationships, that attends to appropriate skill mix and that
facilitates innovation and risk-taking. Both the care processes
and the care environment are made possible by the pre-requisite
attributes of the nurses: professional competence, developed
interpersonal skills, commitment to the job, clarity of beliefs
and values, and a good knowledge of self (5).
Components of the Person-Centered Nursing Framework
(5)
Procedure
The overall goal of the workshops was to begin a practice
culture change which would result in evidence of more person-centered
care practices. The objectives were (5):
• To promote an awareness and understanding of person-centered
nursing
• To articulate explicit values and beliefs that inform
the provision of nursing care
• To develop a shared vision that promotes person-centered
nursing practice
• To collect information on the quality of resident and
staff nurse experience in order to benchmark practice change
• To identify areas for practice change
The workshops were facilitated once a week over four consecutive
weeks. Participants included head nurses and nursing supervisors
of two long term care facilities and a newly opened community
care facility for assisted living. There were 23 participants
in all. Attendance at each workshop varied from 23 to 16.
A focus group was conducted with participants from one of
the long term care facilities 12 weeks later to evaluate the
outcomes in practice. Written consent was received from all
participants in the focus group.
Nurse leaders were targeted as participants with the expectation
that they would become facilitators of practice change on
their units. The workshops utilized creative ways of unleashing
the nurses' leadership potential. By co-creating a shared
vision for care, and critically reflecting on care practices,
they moved a step toward developing a culture of person-centered
care. During the final workshop, they agreed on one priority
area for change. They clearly identified the problem, and
brainstormed on an action plan for change. The nurses were
enabled to use the action learning cycle, to critically reflect
on their work and work environment and to develop alternative
ways of thinking and doing that would enhance quality of life
and satisfaction for residents and families.
The first workshop introduced the participants to the concept
of person-centeredness and the person-centered care framework.
An activity called "Victorian Parlour Game" (7)
was used to help participants recognize empathy for the residents
under their care. In this activity, participants were asked
to think about the question: "if I were one of my residents,
how would I feel right now?" The answers of all the participants
were then organized into an insightful poem that indicated
that each participant was aware of the feelings of isolation,
loneliness and hopelessness often felt by residents of elder
long term care. (See "In Long Term Care")
In small groups, participants mapped aspects of a case study
against the person-centered framework. After plenary discussion
of this activity, participants discussed in pairs how these
concepts could be used to change some practices on their units,
and decided on three ways that they could use these ideas
in their practice in the coming week.
In the second workshop, participants reflected on their individual
values and shared these with one other person in the group.
Then they worked with others from the same nursing unit to
agree on a common set of values and write a shared vision
of nursing care in their unit using the following headings:
• We believe the purpose of our nursing care is...
• We believe this purpose can be achieved by...
• The factors that will help us achieve this purpose
are...
• Other values and beliefs about nursing in our unit
are...
The groups then created a poster depicting their vision and
developed a plan for sharing this with their staff in the
coming week. As preparation for the next workshop, they were
asked to observe care on their unit in the coming week and
note one instance of care that was in keeping with the vision,
and one that did not fit with the vision.
During the third workshop participants evaluated the quality
of the patient-centered processes on their units by comparing
their observations of care with the vision that they had developed
and identifying sources of data for evaluating practice. Using
a provided set of questions to guide their reflection on each
of the person-centered processes, unit groups were asked to
evaluate the quality of care on their units. They then brainstormed
how they could validate these evaluations by using sources
of data available to them. Each group developed a plan for
evaluating the use of person-centered processes on their unit
and for identifying areas of practice that needed to change.
The final workshop examined the attributes of the nurse and
the care environment that are essential for a person-centered
culture of care. It also aimed to assist participants to plan
for a continuous trend toward a person-centered culture of
care. In their unit groups, participants evaluated the context
of care in their facility and discussed how the care environment
contributes to the areas of care that they had identified
for change. Plenary discussion identified and prioritized
common themes related to change to the care context.
The top priority theme was then analyzed by the group to clarify
the problem, identify the evidence of the problem, suggest
desired outcomes, develop possible solutions, and decide on
how outcomes could be evaluated. The action learning cycle
(plan, act, observe, reflect) was presented as a process for
ensuring continuous change in the care culture.
By engaging nursing leaders in reflecting on their practice
settings and comparing what they see with the visions that
they have developed, these workshops initiated a process of
change toward more person-centered
care. Identification of one priority area of change, and employment
of the action learning cycle created the opportunity for the
change process to be sustained.
Evaluation
An evaluation form was completed by participants at the end
of each workshop. Participants commented: "have started
(a change process) and will continue"; "very, very
much excited (to initiate a change in care practices)".
Responses to the evaluation questions indicated that participants
understood the concepts from the workshop, and were able to
identify significant sources of data for evaluating care practices
on their units. Many participants identified incongruence
between care being provided on the units and their shared
vision: "care is task centered" and "nurses
do not spend time talking with residents". They recognized
methods for gathering data on the care processes on their
units including: talk with the residents and let them tell
their stories; patient satisfaction survey; observation; asking
questions; random visits; interviews with the residents and
families; getting feedback from staff. The participants' high
level of engagement in the unit group work as well as the
plenary discussion indicated that the workshops were relevant
to them. They commented after each workshop that they had
enjoyed and learned from each session.
In order to evaluate the usefulness of the workshops in starting
a process of change, a focus group was conducted at one of
the participating long term care facilities 12 weeks after
the workshops were completed. The purpose was to ascertain
if indeed practice change had occurred that would provide
greater quality of life and satisfaction for residents and
families.
Focus group comments indicated that practice change related
to individualized care, inclusion of residents and families
in care decisions, and improved services to residents and
families had indeed occurred. Admission assessment forms had
been modified to include more information about residents'
likes and dislikes, preferred activities, hobbies, etc. and
individualized care plans were developed based on these preferences.
Copies of the care plans were shared with families as well
as the interdisciplinary team. Interests of family members
were being noted and families were included in activities
on the units. Recognizing the desire of one resident to be
involved in meal preparation, opportunities to help prepare
meals for her family were provided, and a weekly cooking activity
was made available to all residents.
A committee had been established to plan activities for residents
and more activities were offered in the afternoon and evening
to accommodate family participation. A volunteer visitor program
provided residents with greater variety in interaction as
well as companionship.
Nurses noted that residents were "more cheerful"
and more active participants in their care. One nurse commented
that resident/staff relationships were stronger. Nurses said
that family members, too, indicated that they appreciated
the extra attention.
Change did not come without some challenges. Nurses noted
that it had been difficult to readjust care routines to accommodate
resident preferences. There were on-going efforts to educate
all staff about the unit vision through making it visible
on posters throughout the facility and communicating it consistently
at monthly unit meetings. The vision had also been published
in both Arabic and English in the form of a handbook, an information
booklet and a poster at the bedside along with the resident
bill of rights.
Nurses also commented that the atmosphere at work had become
more positive and that staff felt informed and involved in
the changes being instituted. They felt that the challenge
now was to increase the momentum of the change and to gain
a reputation as a superior place to work.
Conclusion
Focus group comments indicated that a culture change was happening
in this long-term care facility and that resident care was
becoming more person-centered as outcomes of the workshops.
In this case, a work environment that allowed nurses the freedom
to create a unified vision for care and to recognize and change
practices that did not conform to the vision resulted in greater
satisfaction and quality of life for both nurses and residents.
This paper has described an educational program for nurse
leaders in long term care intended to generate a work culture
change to support the practice of person centered care. More
research into the implementation of care models that support
Arab religious and family values is essential to meet the
growing need for high quality long term residential care in
the Arab Gulf region.
|
In Long Term Care
Longing for compassion and loving care
For feelings of belonging
And the hugs and kisses that is sweet
Lonely and useless
Frustrated and sometimes afraid
They pity me
Such boredom, sadness and loneliness
But even though I am sick I am in safe hands
Anxious but
If my parents are around, beautiful the life is
Need for much attention and love
The time is too long: nothing to do
Bored and depressed
Rejected, alone, pitiful, powerless, depressed
I want to be with my family right now
The touch of their caress, the smile on their faces
Their voice saying how much they love me
Repulsed by wound exudates and smell
Pain but
Life here is better than at my house
Cannot express my feelings
Useless, wasted, a burden to society
They deal with me as an object not
A human being
Machine centered care
Upset and irritable
Lonely and irritable
Thank God for what and who I am
I will overcome and use the best of my abilities
To survive.
|
References
1. El-Haddad, Y. Major trends affecting families in the Gulf
countries 2003. http://www.un.org/esa/socdev/family/Publications/mtelhaddad.pdf
2. Sinunu M., Yount K., El Afify N. Informal and formal long-term
care for frail older adults in
Cairo, Egypt: Family caregiving decisions in a context of
social change. J Cross Cult Gerontol 2009; 24: 63-76.
3. Margolis S, Reed, R. Institutionalized older adults in
a health district in the United Arab Emirates: Health status
and utilization rate. Gerontology 2001; 47: 161-167.
4. Al-Shammari S, Felemban F, Jarallah J, El-Shabrawy A, Al-Bilali
S, Hamad J. Culturally acceptable health care services for
Saudi's elderly population: the decision-makers perception.
Int J Health Plan Manage 1995; 10: 129-138.
5. McCormack B, McCance T. Person-centered nursing: Theory
and practice. Oxford, U. K.: Wiley-Blackwell; 2010.
6. McCormack B, Dewing J, McCance T. Developing person-centered
care: Addressing contextual challenges through practice development.
Online J Issues in Nursing 2011;16(2):1-
7. Nisker, J. Narrative ethics in health care. In Storch J,
Rodney P, Starzonski R. eds. Toward a moral horizon: Nursing
ethics for leadership and practice. Toronto: Prentice-Hall;
2004.
|
 |




