| |
August
2013 - Volume 7, Issue 4
Impact of language
barrier on quality of nursing care at Armed Forces Hospitals,
Taif, Saudi Arabia

|
 ( (
|
Sameer Al-Harasis
Correspondence:
Sameer Al-Harasis, BSN,
RN ,Diploma (Nurse Tutor)
Nursing Clinical Instructor
Armed Forces Hospitals, Taif, Saudi Arabia
Email: shrasis1967@yahoo.com
|
 |
|
Abstract
Since Saudi Arabia has a shortage of nursing staff and
depends on expatriate nurses, difficulties in communication
because of language barriers may affect patient satisfaction
or at the worst may lead to healthcare errors. Objectives:
To determine the effect of language barriers on quality
of nursing care at Taif Armed Forces Hospitals and to
suggest possible interventions to mitigate the effect
of language barriers on quality of nursing care. Methods:
This study was conducted in Armed Forces Hospitals,
Taif Region. Two different questionnaires were applied
(one for nurses in English and the other for admitted
patients in Arabic). Total number of respondents was
343 nurses. Results: Forty-nine percent of the nurses
reported they have difficulty in dealing with patients
because of the language barrier. Healthcare outcomes
that were affected because of language barriers include
general nursing care, understanding patients' needs,
communication with patients, healthcare errors, having
trust in nursing care and feeling satisfaction). An
equal percentage of nurses and patients (90% and 89.5%,
respectively) suggested that attending an Arabic course
during the orientation period is very essential. Conclusion:
Future research is required to determine the effectiveness
of suggested interventions (e.g., Arabic language courses,
bilingual staff, common words dictionary, etc) and their
impact on improving communication (i.e., access to care),
change behaviors (i.e., health outcomes), and ultimately
reduce diseases. Moreover, it is necessary to view the
language barrier through a cultural competency model.
Key words: language, barriers, nurses
|
Introduction
Since Saudi Arabia has a shortage of nursing staff, it depends
on expatriate nurses from foreign countries mainly the Philippines,
India, Malaysia and South Africa. Nurses who came from these
countries are non Arabic speaking resulting in difficulties
in communication between nurses and patients as well as between
nurses and medical staff from other nationalities. Consequently,
these communication problems may affect patient satisfaction
or at the worst may lead to medical errors.
A study conducted in the United Kingdom in 1999 (1) showed
that language barriers may increase the likelihood that a
patient would not return to the same institution for future
care (1). In the United States in 2000, another study showed
an association between language barriers and actual follow-up
appointments (2). Patient compliance is another issue that
emerges from the literature as affected by language access.
Patients who have more difficulty understanding their physician
or nurse would be less likely to follow treatment directions,
and this is not only due to the obvious difficulties in obtaining
accurate information, but also because good communication
can be a source of motivation, reassurance and support, as
well as an opportunity to clarify expectations (3).
Discussing the issue of language barriers is more important
for nurses as they are the only personnel at the patients
bedside twenty four hours a day, seven days a week.
A study in the United States covered eleven Boston area ambulatory
clinics in 2000 showed that language barriers may play a role
in outpatient drug complications, which in turn is related
to lower patient satisfaction. Multiple regression analysis
of the same study revealed that having a primary language
other than English or Spanish was an independent predictor
of patient reported drug complications, along with the number
of medical problems and failure to have side effects explained
before treatment. The level of overall satisfaction was significantly
lower among patients who reported problems related to medication
use than among those who did not (4).
An interview study in an Australian children's Hospital of
parents of Chinese immigrants presenting to the emergency
department, where interviews arre conducted in English, language
barriers and insufficiency of linguistic access services are
significant barriers to care (5).
So it is very important for those working in the healthcare
field and for the decision makers to conduct and support studies
that reveal the impact of language barriers on nursing care
and to look for solutions to overcome drawbacks of this problem
on quality of healthcare and patient satisfaction.
Thus this study was conducted to assess the impact of language
barriers on quality of nursing care at Armed Forces Hospitals,
Taif, Saudi Arabia and to suggest possible interventions to
overcome the effect of language barriers on quality of nursing
care.
Materials and
Methods
This study was conducted during the period from April - December
2009 in Armed Forces Hospitals, Taif, Saudi Arabia. These
hospitals consist of 3 main hospitals (i.e., AlHada, Prince
Mansour and Prince Sultan Hospital) in addition to the Rehabilitation
center. They are serving military personnel and their families
at Taif region.
The study included all nurses working at these hospitals with
a total of 385 nurses distributed in different hospitals.
All nurses who are working at Armed forces hospitals and have
at least one year experience of work in Saudi Arabia at the
beginning of the study were invited to voluntary participate
(n= 360).
A predestined self reporting questionnaire was applied to
all participants. The questionnaire was provided in English
language (the language used by all foreign nurses). It included
socio-demographic information, work experience in and out
of Saudi Arabia, level of reading, writing, speaking and understanding
Arabic, English and other languages, training experiences
in the Arabic language, their attitudes towards impact of
language barrier on quality of healthcare, their experiences
of problems associated with language barriers and their suggestions
to solve the problem.
Another simple questionnaire was distributed to 227 inpatients
already present during the study period. The questionnaire
was in Arabic language and was administered through interview
with the patients. It included questions about the age and
level of education in addition to questions about their assessment
of the magnitude of the language barrier and its relation
to the communication difficulties with the nursing staff as
well its relation to their satisfaction of the healthcare
provided.
Approval of the Research and Ethics committee of the Armed
Forces Hospitals, Taif, Saudi Arabia was obtained to conduct
the study.
Results
This study included 343 nurses with a response rate of 96%
and 227 patients with a response rate of 88%.
The majority of nurses were female (92.7%). There were 58.9%
with nursing high school education, 37.9% bachelor degree
in nursing and only 3.2% with master degree in nursing. The
overall experience in nursing was almost equally distributed
in the following groups: less than 5 years, 5-10 years and
more than 10 years of nursing. More than half of the participating
nurses (56%) have 2-5 years of work in Saudi Arabia including
their work at Taif Armed Forces Hospitals, however, about
20% either had 1-2 years or more than 5 years of work in Saudi
Arabia (Table 1).
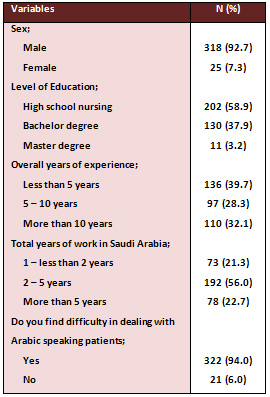
Table 1: Socio-demographic characteristics of the participating
nurses
Regarding patients, there were 120 males out of 227 patients
(55%) and there were 71% among them having less than university
education.
Forty-nine percent of the nurses reported they have difficulty
in dealing with patients because of the language barrier (Table
1).
Regarding Arabic language knowledge, self-report of the participating
nurses revealed that they cannot read or write at all (68.8%
or 70%, respectively). However, 98.5% were either completely
(33.8%) or a little (64.7%) able to speak and 99.7% were either
completely (39.1%) or little (60.6%) able to understand the
Arabic language (Figure 1).
Click here for Figure
1: Level of reading, writing, speaking and understanding the
Arabic language
Almost one fifth of the participating nurses think that healthcare
outcomes (i.e., nursing care, understanding patients' needs,
communication, healthcare errors, having trust in nursing
care and feeling satisfaction) are USUALLY or ALWAYS affected
because of language barriers (median is 22.4%). However, more
than half of the nurses think that the reported healthcare
outcomes are SOMETIMES affected because of language barriers
(median is 55.8%) (Table 2).
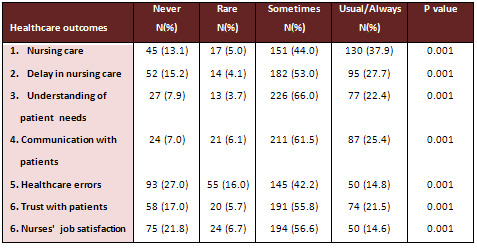
Table 2: Do you think language barrier can affect / lead
to the following healthcare outcomes?
Knowledge of participating nurses about the Arabic language
was estimated using scores 0, 1, 2 for no, little and yes
knowledge of reading, writing, speaking and understanding
as reported by the nurses. It was found that 40.3% of those
who have less than average Arabic language score have experienced
questioning because of language barriers compared to 29.9%
among those who have above average score (p=0.05) (Figure
2).
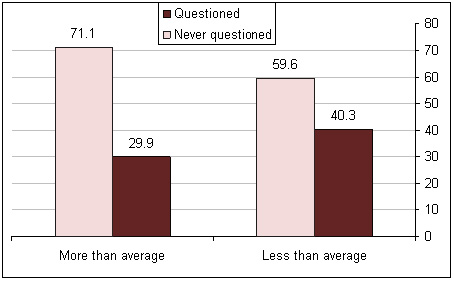
More than average (n= 250) and less than average (n= 93)
p value = 0.05
Figure 2: Previous experience of questioning because of problem
/ mistake related language barrier according to level of Arabic
language knowledge
Among patients, there were 33.2 and 26% who reported communication
difficulties and decreasing satisfaction, respectively, as
usual or always experienced because of language barriers.
Those who reported communication problems and decreasing satisfaction
as sometimes experienced were 59.5% and 56.3%, respectively
(Figure 3).
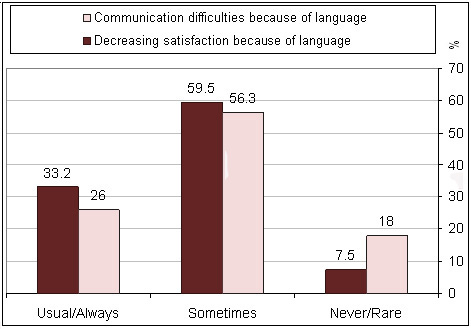
Figure 3: Communication problems and satisfaction of patients
related to language barriers as reported by patients (n=227)
An exactly equal percentage of nurses and patients (90% and
89.5%, respectively) suggested that attending an Arabic course
during the orientation period before starting work is essential.
Similarly, 85% and 83.1%, respectively suggest translators
in different wards to minimize language barriers. However,
94% of nurses compared to 73.9% of patients prefer common
words dictionary as a solution. About 83% of nurses compared
to 64.4% of patients think that using the signal language
can help in minimizing language communication difficulties.
Most of the patients (87.7%) encourage having Arabic speaking
nurses to overcome the problem (Figure 4).
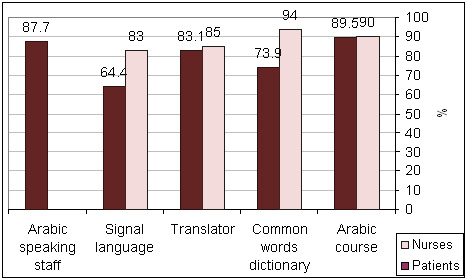
Figure 4: Suggestions of nurses and patients regarding
solutions of language barriers problems
Discussion
Differences in language between healthcare providers and patients
increasingly impose barriers to healthcare (5). The consequences
of language barriers range from miscommunication with its
drawbacks on health outcomes (6) to inefficient use or lack
of access to health care services (7, 8). The current study
may be the first that assesses the magnitude of language barrier
as an obstacle to the healthcare system in the Arab world.
Although the majority of nursing staff in the Arabic speaking
gulf countries are from non-Arabic speaking countries, research
that indulges this major problem are lacking. The current
study revealed that the majority of working nurses find difficulty
in dealing with Arabic speaking patients who represent all
the patients in the facility. Moreover, most of the patients
find difficulties in communication with non-Arabic speaking
nurses and their overall satisfaction is affected.
The current study ranked the healthcare outcomes that may
be affected because of language barriers according to nurses
self-reporting. Understanding of patient needs (88.4%) was
ranked first followed by general communication with patients
(86.9%), quality of nursing care (81.9%), delay in nursing
care (80.7%), building trust with patients (77.3%) and potential
for healthcare errors (57%). Additionally, nurses reported
that language barriers affect the nurses' overall job satisfaction.
A systematic review of 47 articles by Yeo (2004) (9) indicated
that language barriers are associated with lack of awareness
about health care benefits (such as Medicaid eligibility)
(10), less insured status (7), longer visit time per clinic
visit (8), less frequent clinic visits (11), less understanding
of the physician's explanations (6, 12), more lab tests (7),
more emergency room visits (7), less follow-up (8), and less
satisfaction with health services (13, 14). As the reviewed
studies were all observational causal relationship between
language barriers and quality of care could not be established.
Several studies have reported negative associations between
the presence of language barriers and the number of healthcare
visits (10, 11, 15). David and Rhee (1998) (6) concluded that
the language barriers are correlated negatively with patient
satisfaction and medication compliance.
Another literature review by Timmins (2002) (16) showed that
non-English speaking populations lack access to a therapeutic
relationship with their health care provider because of the
language barrier. The patients are at higher risk of health
problems because they do not get benefit from the available
health services. According to that review, language barriers
can lead to poor patient outcomes, increased use of expensive
diagnostic tests, increased use of emergency room services,
poor patient satisfaction and poor or no patient follow-up
when follow-up is indicated.
In research study by Dunn et al (2001), (17) it was concluded
that lack of time and language affected whether a discussion
about cancer screening was required. It was further mentioned
that screening was avoided due to lack of resources for interpretation.
A similar explanation was provided by Thompson and others
(2002) (18) who reported that Hispanics were much less likely
than non-Hispanic whites to ever have had cancer screening
in addition to other socio-demographic factors.
Morales and colleagues (1999) (14) measured dissatisfaction
of patients using five observations about medical staff: (1)
they listen to what patients say; (2) they give answers to
questions; (3) they explain about prescribed medications;
(4) they explain about medical procedures and test results;
and (5) they give reassurance and support. It is worthy of
notice that all these observation require a high quality of
communication and language is usually the core of good communication.
Several studies demonstrate that language barriers result
in both inefficiency and potential increases in costs (7,
8). For instance, Hampers (7) indicates that patients with
language barriers have significantly higher test costs ($145
vs. $105) and longer emergency department stays (165 minutes
vs. 137 minutes) than their English-speaking counterparts.
Kravitz (8) also demonstrated that Spanish- and Russian-speaking
patients averaged 9.1 and 5.6 minutes longer for visits, respectively,
than English-speaking patients.
Various interventions to mitigate the effect of language barriers
on the quality of the provided healthcare have been suggested.
Both nurses and patients in the current study agreed that
administration of Arabic courses for nurses is essential (90%
and 89.5%, respectively). In the US, as the problem is reversed
where patients are non-English speaking, thus they suggested
health education strategies for the patients who do not speak
or read English at the elementary level (19). In such situations
when there is a language barrier, nurses should use simple,
everyday words rather than complex words or medical jargon
(9).
Using nonverbal communication such as hand gestures and facial
expressions has also been suggested by other researchers (6,
7, 8). The percentage of nurses who suggested nonverbal communication
in the current study was higher compared to patients (83%
among nurses vs. 64.4% among patients). Using a dictionary
may be why that is preferred by the patients as it takes time
and may not be suitable in day-to-day communication, however,
for nurses they have it all the time with them and they can
review commonly used words any time.
It is not only attending language classes or using non-verbal
communication; healthcare providers are encouraged to attend
in-services that focus on cultural awareness, especially in
Saudi Arabia where culture is different and affects health
and lifestyle of the population in different ways.
As Saudi Arabia hires healthcare professionals with multicultural
and multilingual backgrounds, assistance from specially trained
interpreters or family members of the patients is essential
to providing enhanced healthcare and culturally competent
care. Having translators in different departments has been
agreed upon by both nurses and patients in the current study
(85% and 83.1%, respectively). The issue of who should be
the interpreter, (whether that person should be a trained
or untrained individual?) has been discussed by Timmins (2002)
(16). An untrained interpreter (i.e., ad hoc interpreter),
can lead to inaccurate communication and ethical breaches
(including role conflicts and patient confidentiality). Using
a family member as an interpreter may not be suitable, especially
when the content is sensitive and disrupts the family relationship.
Suitable interpreters as suggested by Timmins (2002) (16)
include: hiring bilingual healthcare providers, hiring trained
professional interpreters, training volunteer interpreters
from the community and using phone interpreting.
The quality of interpretation depends on many factors including
the accuracy and content of a competent medical interpretation
(20). When untrained personnel are involved in iterpretation
the content of medical advice is often not fully understood
(12) and patients are less satisfied with the health service
(21).
Hiring Arabic speaking staff as an alternative is highly recommended
by the patients, which needs more efforts from healthcare
institutions, decision making, and community leaders to establish
institutions for nursing education and to raise awareness
of the community towards importance and need for Arabic speaking
nurses. This requires a long-term strategy and collaboration
of different organizations.
Proper communication is essential for optimal patient care
and to maintain health.
Future studies may focus on the causal relationship between
language barriers and various health outcomes. Clinical trials
need to be conducted to determine the effectiveness of interventions
(e.g., Arabic language courses, bilingual staff, common words
dictionary, etc) and their impact on improving communication
(i.e., access to care), change behaviors (i.e., health outcomes),
and ultimately reduce disease. Moreover, it is necessary to
view the language barrier through a cultural competency
model. Several conceptual models (22, 23, 24) have been developed;
however, fitting these models to the Arab culture is essential
or developing new fitted models.
References
1- Carrasquillo O,Ovray EJ, Brennan TA, Burstin HR. Impact
of language barriers on
Patient satisfaction in an emergency department. J Gen Internal
Med.1999;14:82-87.
2- www.hc-sc.gc.ca/hcs-sss/pubs/acces/effe-eng.php Accessed
6/4/2008.
3- Betancourt JR, Carrillo JE, Green AR. Hypertension in multicultural
and minority populations: linking communication to compliance.
Curr Hypertens. 1999. Rep., 1, 482-488.
4-Ghandi TK, Burstin HR,Cook EF. Drug complications in outpatients.
J Internal Med.2000;15:149-154.
5- Chak S, Nixonj, Dugdale A. Primary health care for Indo-Chinese
children in Australia. Australian ped J.1984;20:57-58.
6. David RA, Rhee M. The impact of language as a barrier to
effective healthcare in an underserved urban Hispanic community.
Mount Sinai Journal of Medicine. 1998; 65, 393-397.
7. HampersLC, Cha S, Gutglass DJ, Binns HJ, Krug SE. Language
barriers and resource utilization in a pediatric emergency
department. Pediatrics. 1999,
103(6 Pt 1), 1253-1256.
8. Kravitz RL, Helms LJ, Azari R, Antonius D, Melnikow J.
Comparing the use of physician time and health care resources
among patients speaking English, Spanish, and Russian. Medical
Care. 2000, 38, 728-738.
9. Yeo Seonae. Language Barriers and Access to Care. Annual
Review of Nursing Research. 2004, 22 (1), 2004: 59-73(15)
10. Feinberg E, Swartz K, Zaslavsky AM, Gardner J, Walker
DK. Language proficiency and the enrollment of Medicaid-eligible
children in publicly funded health insurance programs. Maternal
and Child Health J. 2000, 6(1), 5-18.
11. Derose KP, Baker DW. Limited English proficiency and Latinos'
use of physician services. Medical Care Research and Review.
2000, 57(1), 76-91.
12. Gerrish K. The nature and effect of communication difficulties
arising from
interactions between district nurses and South Asian patients
and their carers.
Journal of Advanced Nursing. 2001, 33, 566-574.
13. Meredith L, Stewart M, Brown JB. Patient-centered communication
scoring method report on nine coded interviews [Comment].
Health Communication. 2001, 13(1), 19-31.
14. Morales LS, Cunningham WE, Brown JA, Liu H, Hays RD. Are
Latinos less satisfied with communication by health care providers?
Journal of General Internal Medicine. 1999, 14, 409-417.
15. Jacobs EA, Lauderdale DS, Meltzer D, Shorey JM, Levinson
W, Thisted RA. Impact of interpreter services on delivery
of health care to limited-English-proficient patients. Journal
of General Internal Medicine. 2001, 16, 468-474.
16. Timmins CL. The impact of language barriers on the health
care of Latinos in the United States: A review of the literature
and guidelines for practice. Journal of Midwifery and Women's
Health. 2002, 47(2), 80-90.
17. Dunn AS, Shridharani KV, LouW, Bernstein J, Horowitz CR.
(2001). Physician-patient discussions of controversial cancer
screening tests. American J Prev Med. 2001, 20(2),130-133.
18. Thompson B, Coronado GD, Solomon CC, McClerran DF, Neuhouser
ML, Feng Z. Cancer prevention behaviors and socioeconomic
status among Hispanics and non Hispanic Whites in a rural
population in the United States. Cancer Causes & Control.
2002, 13, 719-728.
19. Aboul-Enein FH, Ahmed F. How language barriers impact
patient care: a commentary. Journal of Cultural Diversity.
Fall 2006, 13 (3): 168-9.
20. Woloshin S, Schwartz LM, Katz SJ, Welch HG. Is language
a barrier to the use of preventive services? Journal of General
Internal Medicine. 1997,12, 472-477.
21. Lee LJ, Batal HA, Maselli JH, Kutner JS. Effect of Spanish
interpretation method on patient satisfaction in an urban
walk-in clinic. Journal of General Internal Medicine. 2002,
17, 641-645.
22. Brach C, Fraser I. Can cultural competency reduce racial
and ethnic health
disparities? A review and conceptual model. Medical Care Research
and Review. 2000,
57(Suppl 1), 181-217.
23. Andersen RM. Revisiting the behavioral model and access
to medical care:
Does it matter? J Health and Social Behavior. 1995, 36(1),
1-10.
24. Andersen RM, Rice TM, Kominski GF. Changing the U.S. health
care system: Key issues in health services, policy, and management.
San Francisco:
Jossey-Bass. 2001.
|
 |




