| |
November
2014
- Volume 8, Issue 4
Chemotherapy
safe handling: policy analysis

|
 ( (
|
Mohammad G. H. Tuffaha (1)
Majd. T. Mrayyan (2)
(1) Hashemite University,
School of Nursing, Zarqa, Jordan
(2) Al-Bashir Hospital, Department of Hematology, Amman,
Jordan
Correspondence:
Mohammad G.H Tuffaha
Hashemite University, School of Nursing, Zarqa, Jordan
Email: mohammad_toffaha@yahoo.com
|
 |
|
Abstract
Chemotherapy has an important role in cancer treatment.
The National Institute for Occupational Safety and Health
categorizes chemotherapy as hazardous drugs. Hazardous
drugs pose a potential health risk to personnel who
prepare, handle, administer, and dispose of these drugs.
Chemotherapeutic agents pose any one of the following
characteristics: genotoxicity, carcinogenicity, teratogenicity,
or fertility impairment. The risk for exposure-related
cancers is increased in health care workers who handle
chemotherapy and in female health care workers who become
pregnant; there are also the potential hazards of spontaneous
abortions, stillbirths, and teratogenic effects on unborn
fetuses. Patients receiving chemotherapy and their family
members, can also be exposed to the hazards of chemotherapy
drugs when they handle contaminated equipment or body
fluids. Several studies carried out at hospital units
have shown detectable levels of cytotoxic agents in
the air, on surfaces,
on gloves, and on different parts of the body. The presence
of these drugs in the urine of hospital personnel has
been widely studied. Thus, it is important for everyone
who prepares, handles, administers, and disposes of
chemotherapeutic agents to review and analyze the policy
of safe handling of cancer chemotherapy drugs and waste.
Key words: chemotherapy,
safe, administration, policy, analysis.
|
Introduction
Health policy is defined as a set course of action undertaken
by governments or health care organizations to obtain a desired
outcome (Cherry & Jacob, 2007).
Health policy analysis is defined as an interdisciplinary
approach that analyzes current health policy and proposes
various alternatives for developing future health policy without
pushing a single solution set - rather, it considers the perspectives
of economics, political science, management, communications,
technology, and public health (McLaughlin & McLaughlin,
2008).
Chemotherapy has an important role in cancer treatment (Green
et al., 2009). The National Institute for Occupational Safety
and Health (NIOSH, 2004) has categorized chemotherapy as hazardous
drugs. Hazardous drugs pose a potential health risk to personnel
who prepare, handle, administer, and dispose of these drugs
(Itano & Toka, 2005).
Some patients who have been cured of cancer develop secondary
malignancies believed to be linked to exposure to their initial
chemotherapy regimen. If patients receiving potentially curative
chemotherapy are at increased risk of developing secondary
cancers, what is the risk to health care workers who prepare
and administer these agents? (Green et al., 2009). Although
health care workers are exposed to much lower doses than cancer
patients are, low-dose exposure over long periods can have
long-term health effects (Moretti et al., 2011).
Potential routes of exposure are: 1- direct contact - skin
and mucus membrane contact and absorption, inhalation, or
ingestion (e.g., contaminated food), accidental needle stick.
2- Indirect contact - body fluids and excreta of clients who
have received antineoplastic agents within the past 48 hours
(Itano et al., 2005).
Significantly higher frequency of DNA damage - has been analyzed
using the alkaline single cell gel electrophoresis technique
(comet assay) - in lymphocytes of nurses handling antineoplastic
drugs compared to unexposed controls; the DNA damage was,
however, found to be significantly lower in nurses using compulsory
personal protection equipment during their work (Moretti et
al., 2011).
Thus, it is important for everyone who prepares, handles,
administers, and disposes of chemotherapeutic agents to review
and analyze the policy of safe handling of cancer chemotherapy
drugs and waste.
Step 1
Verify, define and detail the problem
Issue statement
Does the policy of safe handling of cancer chemotherapy drugs
and waste in Albashir hospital provide a safe environment
and prevent hazardous effects to health care workers?
Scope of problem
Chemotherapeutic agents pose a potential health risk to personnel
who prepare, handle, administer, and dispose of these drugs;
chemotherapeutic agents pose any one of the following characteristics:
genotoxicity, carcinogenicity, teratogenicity, or fertility
impairment (Itano, Toka, 2005).
Chemotherapy, because of its relatively narrow therapeutic
index, is often associated with a greater risk of adverse
events (AEs) than other medications, and when used in combination,
may result in an even greater incidence of AEs (Goodin et
al., 2011). Potential effects of exposure to hazardous drugs:
1- short term- occur within hours or days after exposure:
contact dermatitis, alopecia, local skin or mucus membrane
irritation, blurred vision, allergic response, dizziness,
gastrointestinal (GI) tract problems, headache. 2- Long term-
occur within months or years after exposure: liver damage,
chromosomal abnormalities, increased risk of cancer, reproductive
risks (Itano et al., 2005). Green et al., (2009) reported
that the risk for exposure-related cancers increased in health
care workers who handle chemotherapy and in female health
care workers who become pregnant; there are also the potential
hazards of spontaneous abortions, stillbirths, and teratogenicity
effects on unborn fetuses. Patients receiving chemotherapy
and their family members can also be exposed to the hazards
of chemotherapy drugs when they handle contaminated equipment
or body fluids (CNSA, 2003). Several studies carried out at
hospital units have shown detectable levels of cytotoxic agents
in the air, on surfaces, on gloves, and on different parts
of the body. The presence of these drugs in the urine of hospital
personnel has been widely studied. This has led several organizations
to develop guidelines or recommendations with the aim to improve
safety during the handling of antineoplastic drugs and reduce
risk of contamination in the workplace (Moretti et al., 2011).
In addition chemotherapeutic agents may be used for diseases
other than cancer, such as Lupus, and multiple sclerosis.
In some hospitals these drugs are being administered by nurses
without proper training or being chemotherapy certified which
may increase exposure to chemotherapeutic agents for healthcare
providers (Polovich, 2004). Many institutions introduced and
implemented policies and procedures designed to minimize occupational
exposure and consequent risks associated with handling cytotoxic
drugs including economic impact. Health care institutions
would have to value the significant expense to comply with
this policy and the real cost must be weighed against the
potential high cost of the treatment of the health care workers.
No relevant policy analysis was found regarding safe handling
of chemotherapy.
Search resources and associated search terms were Science
Direct Database, PubMed, and Google scholar, using keywords:
chemotherapy, safe handling, policy, cancer, hazardous drugs,
in multiple combinations.
Purpose
This paper aimed to provide policy analysis for safe handling
of cancer chemotherapy drugs and waste in one governmental
educational hospital (Albashir hospital) in order to identify
issues and propose alternative solutions, alternative policy
recommendations for this issue by using a six-step policy
analysis model which will verify and define the problem through
implementing, monitoring and evaluating this policy.
Hospital administrative staff may refuse the change because
of the persistent nursing shortage problem, inability of the
health ministry to hire additional numbers of staff, the change
requires more staff, and the cabinet for the preparation of
chemotherapy is not accommodated in the hematology department.
One of the alternatives is to specialize a room for chemotherapy
preparation. A containing safety cabinet is not necessary
to be in the same department if it is not accommodated, so
there is an urgent need to seek the help of Biomedical Engineering
and Architecture staff, and to put this issue as first priority
for administrative staff; it could be near the department.
If policy of safe handling of cancer chemotherapy drugs and
waste is not applied excellently and with great caution, the
health care workers and even health care institutions will
be in fear of unsafe handling of chemotherapy drugs and waste
mentioned previously in this paper. Consequences of chemotherapy
unsafe handling will affect primarily the patients; and delay
may occur and affect nurses and health care institutions,
therefore there is need to improve the safety of the work
environment; make available protective equipment; develop
standard practice guidelines for oncology nurses; and equipment
(such as cytotoxic drug safety cabinets).
All people who are affected by unsafe handling of chemotherapy
directly or indirectly are concerned in this policy analysis.
The government, healthcare institutions, healthcare professional/workers,
and patients and their families. The government (Ministry
of Health) have to fund health care institutions to make a
safe environment for safe handling of chemotherapy including
safety cabinet in specialized room and also have to hire additional
numbers of staff. The health care institution has the responsibility
to adopt policies that respond to the needs of patients and
health care workers, and maintain the physical environment,
patient and staff education and training.
Health care workers have to update their information regarding
chemotherapy and safe handling and to seek a safe environment
and specialized equipment for the preparation of chemotherapy
and disposal of waste.
Step 2
The purpose of the policy is to delineate appropriate handling
of cytotoxic agents and safe dealing and handling of its waste
products, in addition to ensuring quality patient care and
optimal occupational safety during the administration of chemotherapy
drugs. It is the policy of the radiotherapy department to
apply best safety practice in handling of cytotoxic agents
and its waste products to assure staff, and patient safety.
Policy will be evaluated in terms of administrative ease,
costs and benefits, effectiveness, equity, legality, and policy
acceptability. The desirable outcomes are providing new recommendations
for stakeholders and to be applied and hence ensure safe practice
and build a safe environment in the whole health care institution.
The undesirable outcomes are resistance to change by health
care workers; they not aware of the importance and seriousness
of safe handling of chemotherapy, and the inability to assign
more staff in the oncology department by health care institutions
because the alternatives will cost them.
Safe handling of cancer chemotherapy drugs and waste policy
is clearly stated in terms of purpose, values, and responsibility,
definitions, and guidelines, and mostly covers all safety
practices, is relatively easy to administer, is cost effective,
is not equal for all departments, is legal and accepted but
not easily accessible.
Step 3
The policy mostly covers all safety practices, but need to
be comprehensive, clear, unified for all departments, and
some aspects must be added because of their importance.
The alternatives are: a) unify the policy for departments
dealing with chemotherapy, mainly radiotherapy/medical oncology
department (solid tumor) and hematology floor, b) safety cabinet
in specialized room for chemotherapy preparation in hematology
floor, c) that chemotherapy should be administered only in
oncology departments even for non-cancer patient, d) RNs who
didn't receive specific education and training regarding chemotherapy
are not privileged to deal with chemotherapy.
Experts from Albashir hospital were consulted. Most of them
showed acceptance and interest. It's planned to propose and
consult on this policy analysis with the policy development
committee.
But the question again is, does the policy of safe handling
of cancer chemotherapy drugs and waste
in Albashir hospital provide a safe environment and prevent
hazardous effects to health care workers?
Step
4
For the evaluation of the policy we should identify the major
missing factors that lead to occupational hazards in the work
place, and then find the best alternatives that may strengthen
the policy and protect the health care workers from hazards
of unsafe handling of chemotherapy. Chemotherapy is mainly
administered in Albashir hospital in two departments: radiotherapy/
medical oncology department (solid tumors), and in hematology
floor (blood cancers mostly). In the radiotherapy department
there is a safety cabinet in a specialized room where the
preparation is being done, but in the hematology floor there
is no safety cabinet in a specialized room because the safety
cabinet does not accommodate the chemotherapy preparation
room in the new building where the hematology floor is , besides
it is not stated in the policy that chemotherapy preparation
should be in the chemotherapy preparation room inside a safety
cabinet. Also the policy is made for the radiotherapy/medical
oncology department (solid tumor) as mentioned in the definition;
the policy should be the same for departments that deal with
chemotherapy. also during my work I noticed that chemotherapy
is prescribed for non-cancer patients outside the chemotherapy
department ; a real example is once a nurse came to me in
the hematology floor from medical floor and he showed me a
medication (cyclophosphamide) for a patient with Behçet's
disease and he asked me is this chemotherapy? How is this
medication prepared? How is this medication administered?
So we should add to the policy that chemotherapy should be
administered only in the oncology departments even for non-cancer
patients, because in non-oncology departments there is no
specialized chemotherapy preparation room, and non-oncology
nurses didn't know how to deal with chemotherapy safely. Staff
with minimal experience or no experience may be responsible
for handling hazardous drugs in units or areas that do not
normally care for cancer patients with chemotherapy management.
Specific training is required to prepare those staff before
assigning them to such a procedure (Brown et al., 2001). So
we can add to the policy that RNs who have not received specific
education and training regarding chemotherapy are not privileged
to deal with chemotherapy; some local hospitals apply this
point, but it is not clearly stated in their policies. Education
and training should focus on risks of exposure based on strong
evidence from research findings. All these alternatives will
ensure safe handling of chemotherapy.
Click here for Table
1: Appropriate methods of applying alternatives and expected
outcomes
Step 5
Click here for
Table 2: Alternative solution
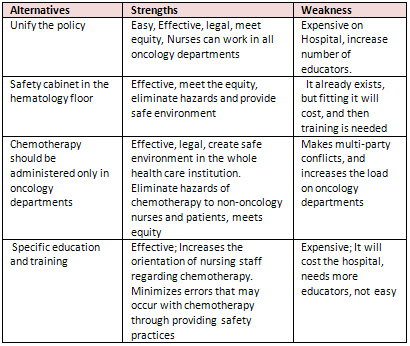
Table 3: Strengths and weakness of each Alternative
Step 6
The main goal of this policy analysis is to provide standardized
guidelines in order to ensure safe handling of cancer chemotherapy
drugs and waste, and to fill the gap in the policy and discuss
and evaluate best alternatives. The plan to implement new
policy is to meet stakeholders in Albashir hospital and convince
them about new recommendations, but before that I will make
a brochure about chemotherapy and risks of exposure and routes
of exposure and emphasizing on the importance and seriousness
of safe handling of cancer chemotherapy drugs and waste, and
then distribute it to all oncology staff, and I will also
distribute for them a draft of a new policy and I will take
their feedback by filling in a questionnaire and the table
of alternative solutions evaluation in terms of administrative
ease, costs and benefits, effectiveness, equity, legality,
and political acceptability. I will work to publish this policy
analysis in a journal to encourage health care workers and
convince stakeholders to consider new solutions. Albashir
hospital stakeholders should have access to the proposed recommendations.
I will recommend to designate a committee of health professionals
as a monitoring system for assuring compliance with the safe
handling of cancer chemotherapy drugs and waste policy, and
check competencies of all oncology staff regarding safe handling
of chemotherapy frequently, monitoring and measuring safe,
quality and ethical services, encouraging staff to report
incidents, not for disciplinary action but for identifying
problems and finding solutions.
I will use the following tables to evaluate the policy; I
will give it to stakeholders and all oncology staff in the
radiotherapy department and hematology department and ask
them to fill in the tables:
Click
here for Table templates
References
Brown, K.A., Esper, P., Kelleher, L.O., O'Neill, J.E.B., Polovich,
M., & White, J.M. (2001). Chemotherapy and biotherapy
guidelines and recommendations for practice. Pittsburgh, PA:
Oncology Nursing Society.
Cherry, B., & Jacob, S.R. (2007). Contemporary nursing:
Issues, trends, & management (3rd ed.). St. Louis: Mosby.
CNSA. (2003). Position statement on the minimum education
and safety requirements for RNs involved in the administration
of cytotoxic drugs, p.1. Retrieved November 2013, from http://www.cnsa.org.au/publications_policies_pub.htm
Goodin, S., Griffith, N., Chen, B., Chuk, K., Daouphars, M.,
Doreau, C., Patel, R.A., Schwartz, R., Tamés, M.J.,
Terkola, R., Vadnais, B., Wright, D., Meier, K. (2011). Safe
Handling of Oral Chemotherapeutic Agents in Clinical Practice:
Recommendations from an International Pharmacy Panel. Journal
of Oncology Practice, 7, (1), 7-12
Green, E., Johnston, M., Trudeau, M., Schwartz, L., Poirier,
S., Macartney, G., Milliken, D. (2009). Safe Handling of Parenteral
Cytotoxics: Recommendations for Ontario. Journal of Oncology
Practice , 5, (5), 245-249
Itano, J.K., & Taoka, K.N. (Eds.). (2005). Core Curriculum
for Oncology Nursing (4th ed.). Pittsburgh, PA: Oncology Nursing
Society.
McLaughlin, C. P., & McLaughlin, C. (2008). Health policy
analysis: An interdisciplinary approach. Sudbury, Mass: Jones
and Bartlett Publishers.
Moretti et al.: A study protocol for the evaluation of occupational
mutagenic/carcinogenic risks in subjects exposed to antineoplastic
drugs: a multicentric project. BMC Public Health 2011 11:195.
National Institute for Occupational Safety and Health (NIOS,
2004). Preventing occupational exposure to anti-neoplastic
and other hazardous drugs in health care settings. Retrieved
October 2013 from http://www.cdc.gov/niosh/docs/2004-165/pdfs/2004-165.pdf
Polovich, M. (2004). Safe handling of hazardous drugs. Online
Journal of Issues in Nursing. 9, (3), 5.
|
 |




